Session Information
Session Type: Abstract Session
Session Time: 4:00PM-4:15PM
Background/Purpose: Hispanic and African American race/ethnicities have been associated with poor COVID-19 outcomes in the general population and in rheumatic disease patients within the COVID-19 Global Rheumatology Alliance (GRA); however, such associations within SLE patients have not been evaluated. The aim of this study is to determine the association between race/ethnicity and COVID-19 outcomes in SLE patients from the US.
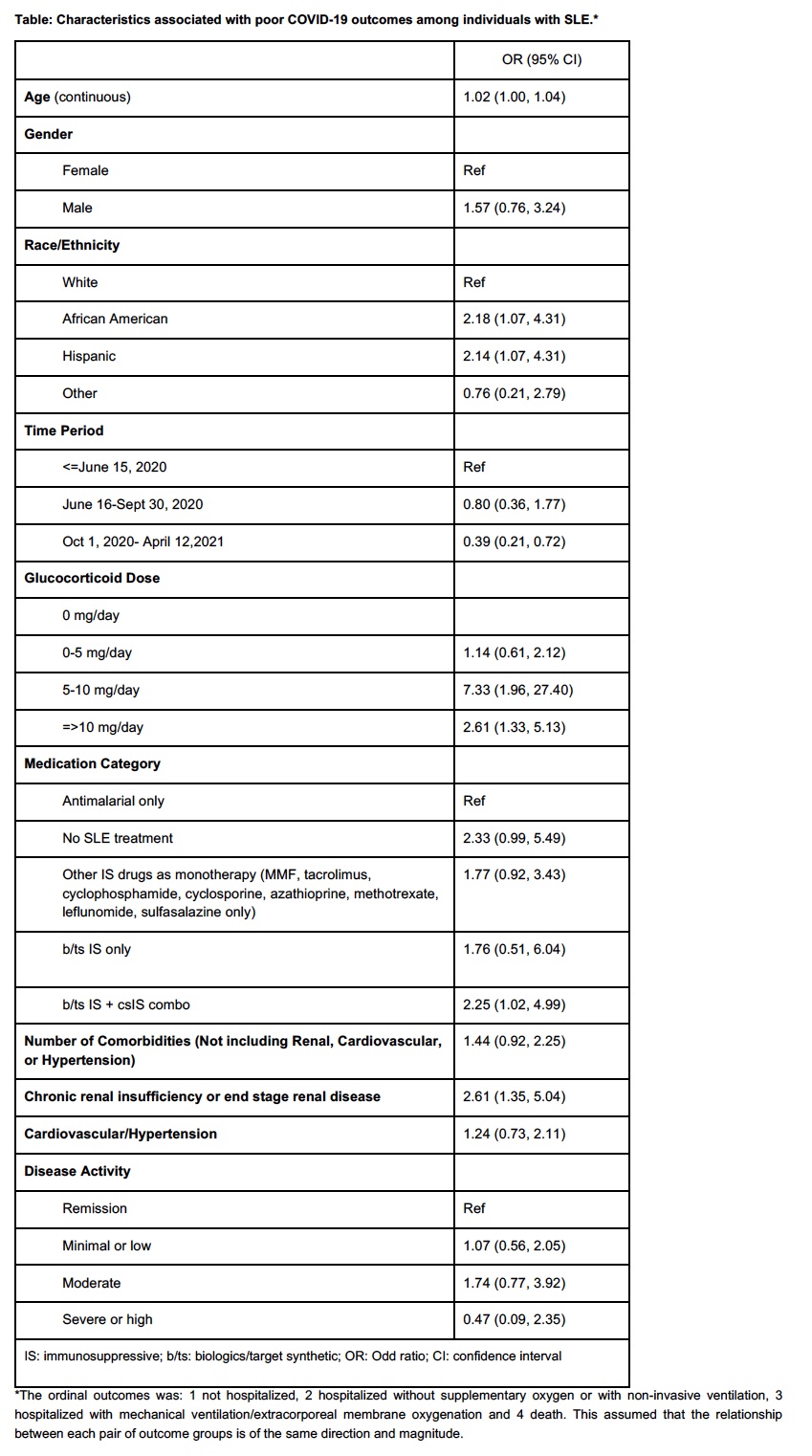
Methods: US SLE patients from the COVID-19 GRA enrolled between March 24th 2020 and April 12th 2021 were studied. Variables included were age, gender, race/ethnicity (White, African American, Hispanic and others), comorbidities (chronic renal disease, cardiovascular disease, and the number of other comorbidities), disease activity (remission, low, moderate, high), time period, glucocorticoid dose, antimalarials and immunosuppressive (IS) drug use. Drugs were categorized into five groups: antimalarials only (reference), no SLE therapy, classic IS drugs monotherapy, biologics/target synthetic IS drugs, and combination therapy. The ordinal outcome categories were: 1. hospitalized without supplementary oxygen and/or not hospitalized, 2. hospitalized with non-invasive ventilation, 3. hospitalized with mechanical ventilation/extracorporeal membrane oxygenation and 4. death. We constructed ordinal logistic regression models evaluating the relationship between COVID-19 severity and race/ethnicity, adjusting for possible confounders.
Results: Five-hundred and four patients were included; 458 (90.9%) were women and the median age was 46.8 (SD: 13.9) years. Four hundred and three (80.0%) patients were not hospitalized; 36 (7.1%) patients were hospitalized without oxygen or with non-invasive ventilation, 49 (9.7%) patients were hospitalized with mechanical ventilation/extracorporeal membrane oxygenation and 16 (3.2%) died. In a multivariable model, African American [OR=2.18 (1.07-4.31)] and Hispanic [OR=2.14 (1.07-4.31)] race/ethnicities were associated with poorer outcomes. Additionally, prednisone-equivalent doses between 5-10 mg/d [OR=7.33 (1.96-27.40)] and >10 mg/d [OR=2.61 (1.33-5.13)], IS drugs (combinations) [OR =2.25 (1.02, 4.99)] and chronic renal disease [OR =2.61 (1.35, 5.04)] were associated with more severe COVID-19 outcomes. COVID-19 diagnosis between October and April 2021 vs. earlier time periods [OR=0.39 (0.21-0.72)] was associated with less severe COVID-19 outcomes (Table 1).
Conclusion: African American and Hispanic individuals with SLE experienced more severe COVID-19 outcomes, which is consistent with findings in the US general population. These results likely reflect socioeconomic and health disparities and suggest that more aggressive efforts are needed to prevent infection in this population.
To cite this abstract in AMA style:
Ugarte-Gil M, Alarcn G, Seet A, Izadi Z, Duarte-Garcia A, Gilbert E, Valenzuela-Almada M, Wise L, Sparks J, Hsu T, D'Silva K, Patel N, Sirotich E, Liew J, Hausmann J, Sufka P, Grainger R, Bhana S, Costello W, Wallace Z, Jacobsohn L, Strangfeld A, Frazão Mateus E, Hyrich K, Gossec L, Carmona L, Lawson-Tovey S, Kearsley-Fleet L, Schaefer M, Machado P, Robinson P, Gianfrancesco M, Yazdany J. Association Between Race/Ethnicity and COVID-19 Outcomes in Systemic Lupus Erythematosus (SLE) in United States Patients: Data from the COVID-19 Global Rheumatology Alliance [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/association-between-race-ethnicity-and-covid-19-outcomes-in-systemic-lupus-erythematosus-sle-in-united-states-patients-data-from-the-covid-19-global-rheumatology-alliance/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/association-between-race-ethnicity-and-covid-19-outcomes-in-systemic-lupus-erythematosus-sle-in-united-states-patients-data-from-the-covid-19-global-rheumatology-alliance/