Session Information
Date: Sunday, November 12, 2023
Title: (0176–0195) Healthcare Disparities in Rheumatology Poster I: Lupus
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Systemic Lupus Erythematosus (SLE) is a heterogenous systemic autoinflammatory disease that disproportionately effects young women and minoritized populations. Disparities are multifactorial with genetic, hormonal, and environmental contributors. Literature has implicated the role of social determinants of health, specifically low individual socioeconomic status (SES) not just with SLE risk, but also cumulative SLE end organ damage due to disease and consequences of therapy. The area deprivation index (ADI) describes neighborhood social risk by integrating 17 census block factors that correlate with many disease outcomes. We hypothesized that patients with incident SLE in more disadvantaged ADI neighborhoods would more rapidly accumulate damage compared to more advantaged ADI groups.
Methods: This observational cohort study included incident SLE patients from three systems representing urban, suburban, and rural patients across one state. Abstractors manually validated incident SLE cases that fulfilled the 1997 American College of Rheumatology (ACR) and 2012 SLE International Collaborating Clinics (SLICC) criteria. Sociodemographic data and diagnoses related to end organ damage through 2020 were manually abstracted. We used the original US ADI publication to produce ADI rank quintiles. Time to damage, as defined by abstracted events of the SLICC/ACR Damage Index, was assessed at SLE diagnosis and through death or study end (12/31/2020). We used Cox regression to estimate survival curves of time to first damage event from SLE diagnosis stratified by ADI to test our hypothesis.
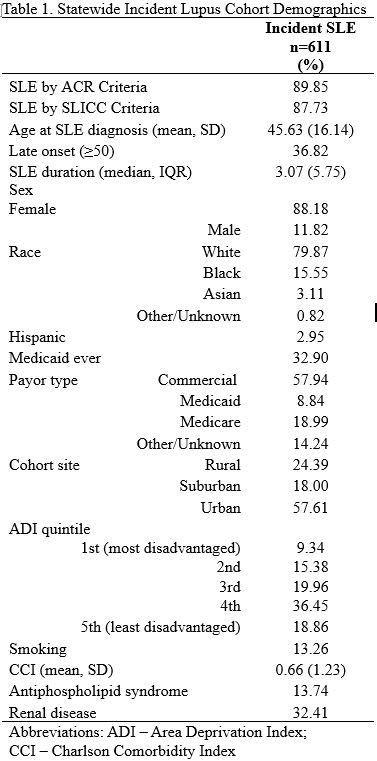
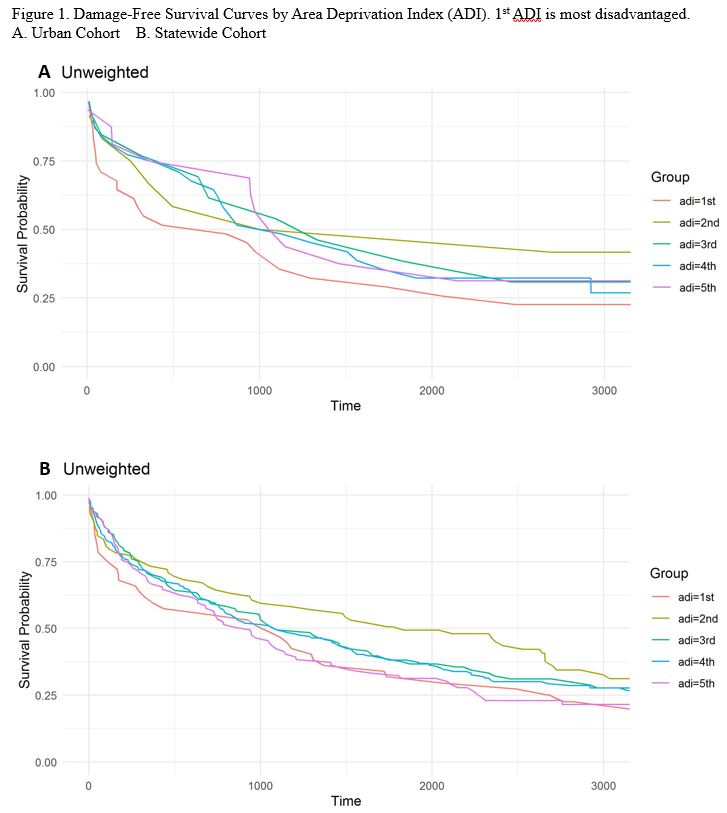
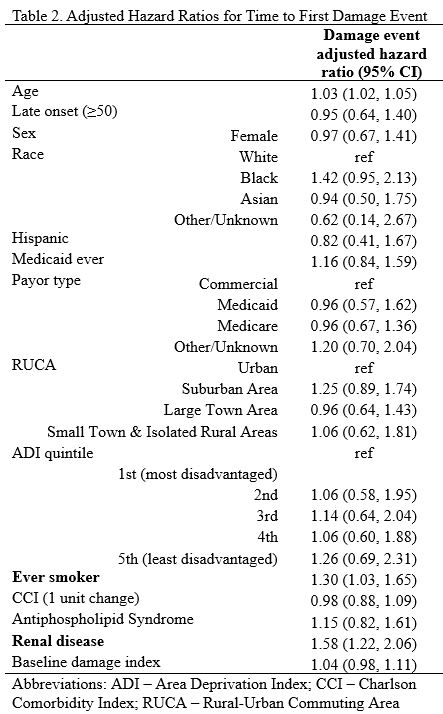
Results: In a total cohort of 611 incident lupus cases, 524 had complete data. Table 1 shows 88% female and 88% White patients with a low proportion in the most disadvantaged US ADI group. Of those in the most disadvantaged ADI, 67% came from the urban system. Figure 1A shows survival curves of patients from the urban system demonstrating a trend of reduced damage-free survival within the most disadvantaged ADI (median 806 days) compared to those more advantaged (least disadvantaged median 1100 days; log rank insignificant). Total cohort survival (Figure 1B) showed no significant association by ADI. Table 2 shows multivariable hazards with no significance by ADI; significance for age, smoking, and baseline renal disease.
Conclusion: While many studies have investigated associations between individual SES and SLE, ours is among the first to investigate the relationship between neighborhood SES, measured by ADI, and damage in incident SLE. In contrast to our hypothesis, ADI was not statistically associated with damage-free survival. The urban cohort demonstrated the expected reduced damage-free survival trend in the most disadvantaged ADI, suggesting high neighborhood disadvantage may impact SLE damage. Limitations include risk of sampling bias with the small sample size of the most disadvantaged ADI group. Furthermore, neighborhood-level factors may be distinct between urban vs non-urban areas; more research is needed to determine if or how neighborhood disadvantage impacts outcomes in SLE.
First ADI is most disadvantaged. A. Urban Cohort B. Statewide Cohort
To cite this abstract in AMA style:
Katz J, Sutherland B, Yu A, Cormier J, Jiang Y, Gazeley D, Elwert F, Bartels C. Association Between Area Deprivation Index and Organ Damage Accumulation in a Statewide Incident Lupus Cohort [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/association-between-area-deprivation-index-and-organ-damage-accumulation-in-a-statewide-incident-lupus-cohort/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/association-between-area-deprivation-index-and-organ-damage-accumulation-in-a-statewide-incident-lupus-cohort/