Session Information
Date: Sunday, November 13, 2016
Title: Rheumatoid Arthritis – Human Etiology and Pathogenesis - Poster I
Session Type: ACR Poster Session A
Session Time: 9:00AM-11:00AM
Methods: Patients (n=106) with newly diagnosed RA according to the ACR 1987 criteria and na•ve to treatment with oral glucocorticoids or DMARDs were included. HRCT was performed in order to assess the presence parenchymal (nodules, ground-glass opacities, fibrosis, emphysema) and airway abnormalities (bronchiectasis, air trapping, air wall thickening). Bronchoscopy was performed on 22 patients to retrieve BAL. EliA system (Phadia) was used to detect RF IgA and IgM, anti-CCP2 IgA and IgG, and ISAC peptide microarray (Phadia) was used to detect antibodies against 10 citrullinated (Cit) peptidic antigens: CCP-1 (Filaggrin), CEP-1 (α-enolase), Vim 2-17, Vim 60-75 (Vimentin), Fib α 36-50, Fib α 573, Fib α 591, Fib α 621-635, Fib β 36-52, Fib β 60-74 (Fibrinogen). Logistic regression analysis was performed to examine associations between HRCT lung changes at the time of RA diagnosis and autoantibodies. Due to the potential risk for effect modification of smoking and its strong association with cit-Abs, we stratified the cohort according to current vs non-smokers.
Results: HRCT parenchymal and airway changes was present in 58 (54.7%) and 68 (64.2%) patients, respectively. The forced vital capacity (FVC) was significantly lower in the presence of airway abnormalities, while the ratio FEV1/FVC was significantly lower in patients with parenchymal lung changes. Higher age, RF IgA, CCP2 IgG, ever smoking and pack-years above 24 were significant predictors of parenchymal lung changes. Some ACPA fine specificities, especially against Cit Fib and Vim peptides, were associated to parenchymal lung changes in ever smokers. The risk of having parenchymal changes increased parallel to the increase in number of ACPA specificities. Having more than 5 ACPA specificities at the time of diagnosis increased the risk of having parenchymal lung abnormalities in current smokers (OR=13.8, 95% CI=1.0-196.2, p=0.05) (Table 1). In the subgroup of patients that underwent bronchoscopy, antibodies against Cit Vim and Fib peptides were detected in the BAL mainly in current smoker (4/9, 45%) and to a lesser extent in non-smokers (3/13, 23%). Patients with Ab positivity in the BAL were also positive for same antibodies in paired serum samples.
Conclusion: The presence of RF IgA, anti-CCP2 IgG and antibodies to Cit Fib and Vim peptides were associated with parenchymal lung changes in early-untreated RA. The more ACPA fine specificities, the higher the risk of having parenchymal lung changes already at the time of RA diagnosis. 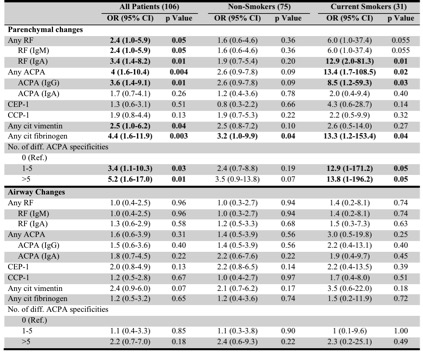
To cite this abstract in AMA style:
Joshua V, Chatzidionysiou K, Reynisdottir G, Hensvold A, Hansson M, Nogueira L, Serre G, Grunewald J, Catrina AI. Association Between ACPA Fine Specificity and High Resolution Computed Tomography Lung Changes in Patients with Early Rheumatoid Arthritis [abstract]. Arthritis Rheumatol. 2016; 68 (suppl 10). https://acrabstracts.org/abstract/association-between-acpa-fine-specificity-and-high-resolution-computed-tomography-lung-changes-in-patients-with-early-rheumatoid-arthritis/. Accessed .« Back to 2016 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/association-between-acpa-fine-specificity-and-high-resolution-computed-tomography-lung-changes-in-patients-with-early-rheumatoid-arthritis/
