Session Information
Date: Sunday, November 12, 2023
Title: (0325–0344) Patient Outcomes, Preferences, & Attitudes Poster I
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Rheumatology outpatients receiving immunosuppressive medications (IS) inevitably develop acute infections. Expert guidance, in accordance with usual clinical practice, recommends counseling patients on “sick day rules.” Patients are recommended to pause IS (with the exception of corticosteroids, which require dose increases) during an acute infection, resuming only when clinically improved. Prior studies have shown poor understanding of “sick day rules” specific to chronic steroid therapy in rheumatology outpatients. [Courtney, 2022]. However, the scope of this problem has not yet been described among the majority of rheumatology outpatients who receive non-steroid IS. Our study aimed to quantify the rate of proper adherence to “sick day rules” in a general rheumatology clinic. We hypothesized that we would find a high rate of non-adherence and illuminate a preventable source of patient harm.
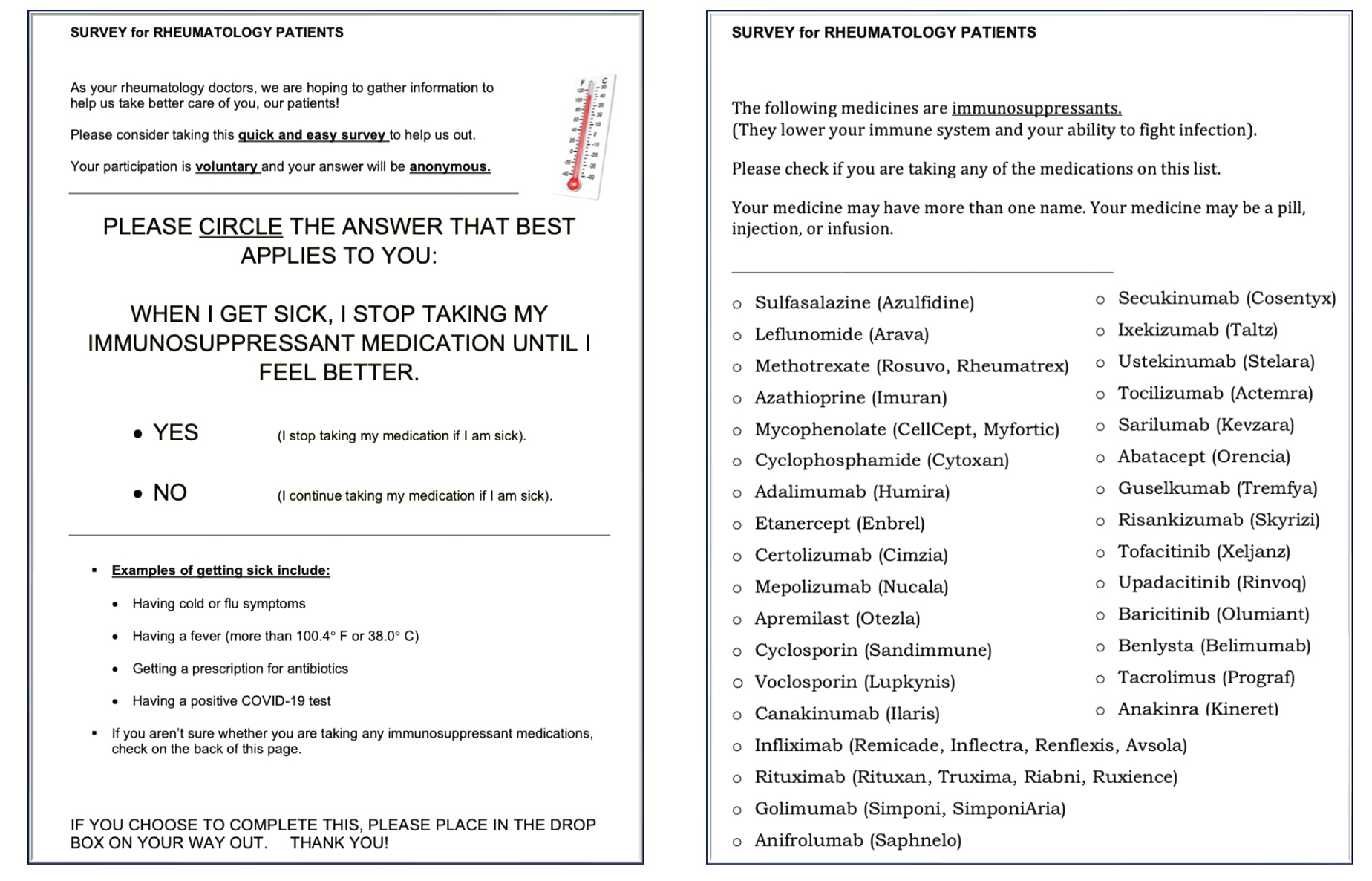
Methods: This was a cross-sectional study of outpatients attending general rheumatology clinic visits in spring 2023. Patients who agreed to participate received the one-page document shown in Figure 1. Patients were asked to respond ‘yes’ or ‘no’ to the statement: “When I get sick, I stop taking my IS until I feel better.” Patients were also asked to select the medications they were currently receiving. Surveys were de-identified. A Spanish-language version of the survey was made available. Any patient currently receiving DMARD therapy was eligible to participate. Exclusion criteria were as follows: no active prescription for a DMARD; active prescription for hydroxychloroquine, colchicine, or corticosteroids only; and inability of the patient (or family member/caregiver present) to read English or Spanish.
Results: 82 patients returned a completed survey. Overall, 32 patients (39%) responded “no,” indicating that they would not interrupt IS if they became ill. 73 of 82 patients indicated which medications they were receiving. Among patients receiving biologic DMARD (bDMARD) therapy, apremilast, or JAK inhibitors, 9 of 37 (24%) responded “no” to the survey question. Among patients receiving only conventional synthetic DMARD (csDMARD) therapy, 21 of 36 (58%) responded “no” to the survey question.
Conclusion: Nearly 40% of the patients in our sample receiving IS indicated non-adherence to recommended “sick day rules.” Among patients receiving only csDMARD therapy, this proportion rose to 58%. As hypothesized, our findings highlight an area for quality improvement and harm reduction. We observed particularly poor understanding among patients receiving csDMARDs only, even though these patients may still be considerably immunosuppressed. Our study was limited the risk of completion bias, potentially lowering the response rate in patients with poorer health literacy and worse disease control. We plan to intensify patient counseling in our clinic, including posting signage throughout our clinic displaying proper “sick day rules.” We will repeat the same survey with a random sample from the same clinic, and we hypothesize that adherence will improve after our intervention.
To cite this abstract in AMA style:
Aksoy M, Gonzalez Manrique P, Greenblatt H, Gilek-Seibert K. Assessment of Patient Adherence to “Sick Day Rules”: A Cross-sectional Study of Rheumatology Outpatients Prescribed Immunosuppressive Medications [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/assessment-of-patient-adherence-to-sick-day-rules-a-cross-sectional-study-of-rheumatology-outpatients-prescribed-immunosuppressive-medications/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/assessment-of-patient-adherence-to-sick-day-rules-a-cross-sectional-study-of-rheumatology-outpatients-prescribed-immunosuppressive-medications/