Session Information
Session Type: Abstract Session
Session Time: 1:00PM-2:30PM
Background/Purpose: In 2023, the American College of Rheumatology published a conditional recommendation for patients living with Rheumatoid Arthritis to follow a “Mediterranean style” diet. However, patient perceptions and potential barriers to implementation of this dietary pattern remain uncharacterized. In this descriptive study, we assessed the adherence and barriers to adoption of the Mediterranean Diet in a racially, culturally, and economically diverse population living with Rheumatoid Arthritis in the United States.
Methods: An online survey was created with questions to assess baseline Mediterranean Diet Adherence Scores (MeDAS), current dietary patterns and preferences, and potential barriers to adoption of the Mediterranean Diet. The study was advertised in Rheumatology clinics across the United States as well as relevant social media accounts from partner patient advocacy organizations including the Arthritis Foundation and The Global Healthy Living Foundation.
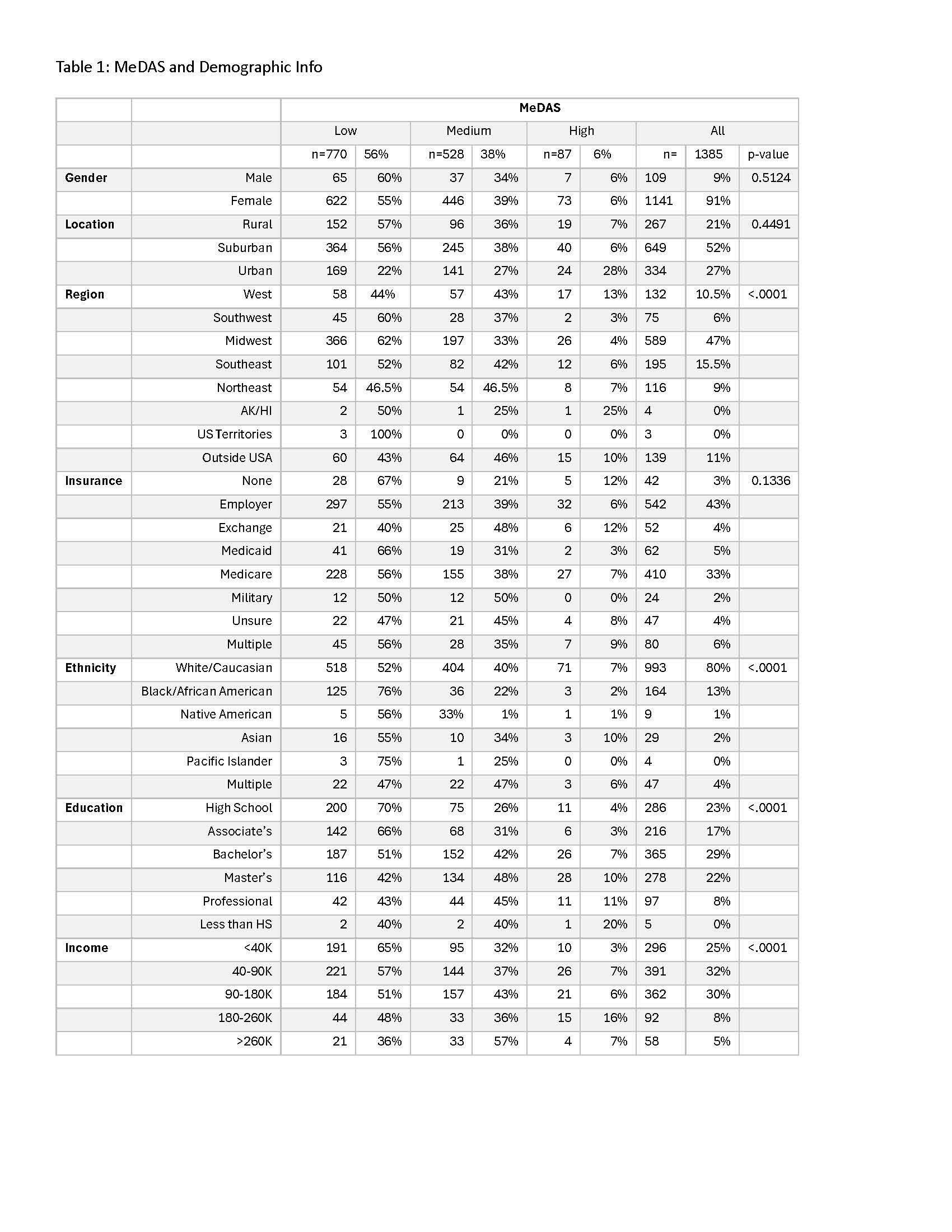
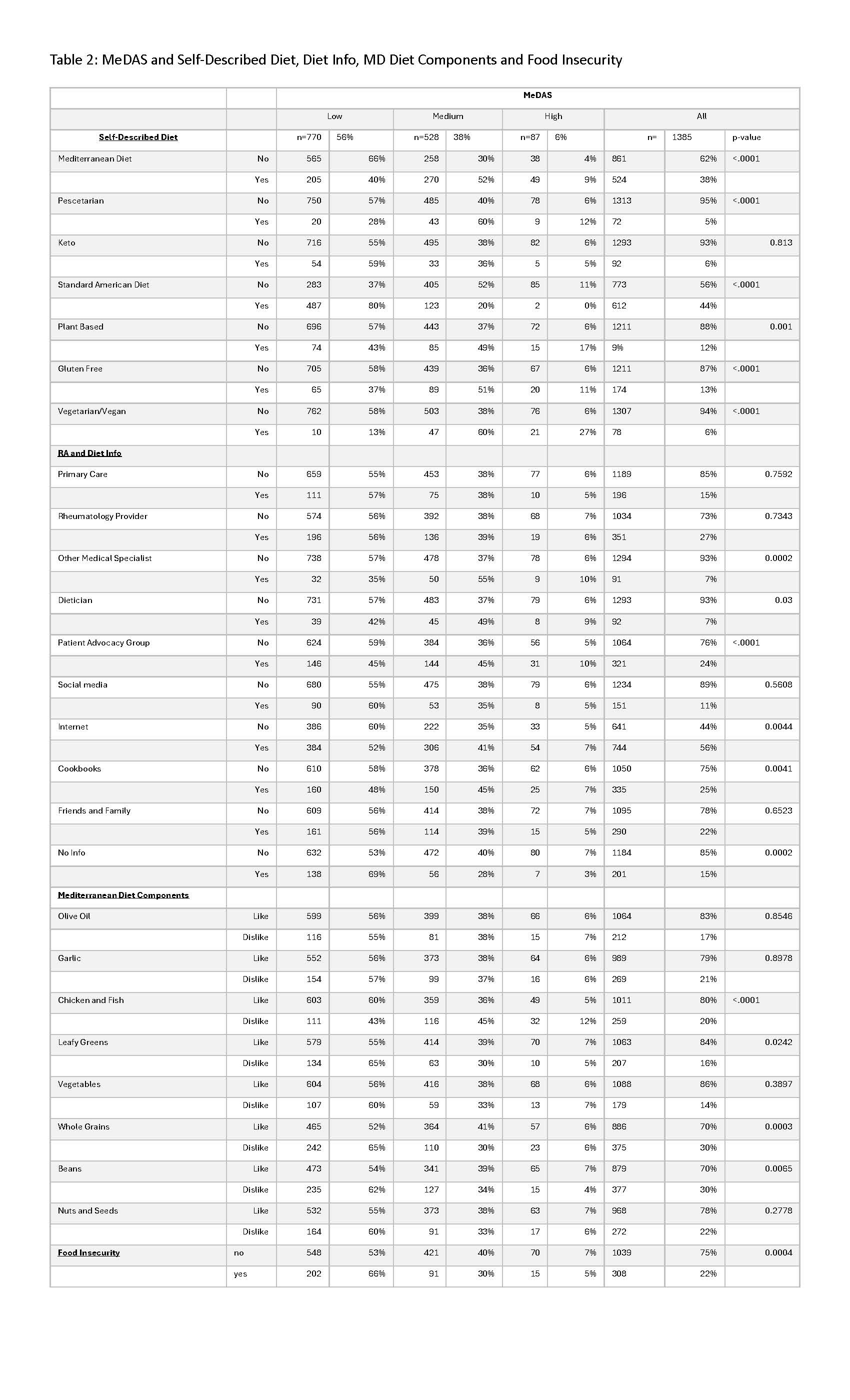
Results: A total of 1,385 respondents with Rheumatoid Arthritis (RA) from across the United States completed the survey. Participants were primarily female (91%), from all regions of the country, and had education and income levels matching the broader US population. Most participants (56%) scored “low” on the MeDAS questionnaire. Approximately 20% of our respondents met screening criteria for food insecurity, and this was significantly associated with low MeDAS. Living in Southern and Midwestern US regions, lower education levels, lower income levels and African American race were significantly associated with lower baseline MeDAS. Self-described vegans and vegetarians had the highest MeDAS, with 27% scoring in the “high” adherence category. Spending less than 60 minutes on meal preparation daily was significantly associated with lower MeDAS. Up to 30% of respondents reported a major food aversion to one or more components of the Mediterranean Diet, with beans (30%) and whole grains (30%) representing the most disliked food categories. Although 84% of respondents were open to trying a Mediterranean style diet as a complementary treatment for their RA, only 27% of respondents reported hearing information about diet and RA from their Rheumatology provider. Those who received information about nutrition from their Rheumatology provider did not have a significantly higher MeDAS. However, those seeking and receiving information about diet and RA from patient advocacy organizations did have significantly higher MeDAS compared to those unfamiliar with these patient facing groups.
Conclusion: Although Americans living with RA from diverse backgrounds are open to additional education regarding a “Mediterranean style” diet, most do not follow this evidence-backed dietary pattern. Food insecurity and food aversions to components of the Mediterranean Diet represent major barriers to implementation. Additionally, most participants did not receive information about a Mediterranean style diet from their rheumatology provider and were not aware of the Mediterranean style diet as a complementary treatment for RA.
To cite this abstract in AMA style:
Thompson C, Ventura i, Edens C, Katsumoto T, Popuri S. Assessing the Feasibility of a Mediterranean-Style Diet for Patients with Rheumatoid Arthritis in a Racially and Culturally Diverse Population Across the United States [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/assessing-the-feasibility-of-a-mediterranean-style-diet-for-patients-with-rheumatoid-arthritis-in-a-racially-and-culturally-diverse-population-across-the-united-states/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/assessing-the-feasibility-of-a-mediterranean-style-diet-for-patients-with-rheumatoid-arthritis-in-a-racially-and-culturally-diverse-population-across-the-united-states/