Session Information
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: Low back pain (LBP) is a leading cause of doctor visits and disability. The annual direct expenditures for LBP management exceed $80 billion, not including indirect costs associated with prolonged disability and lost worker productivity. Despite increasing expenses over time, patient outcomes have not improved, which may be due to overutilization of diagnostic imaging, invasive procedures, and unnecessary specialty referrals. Many providers investigate anatomic structures as an underlying etiology for back pain, which can lead to inappropriate, and even harmful low-validity tests. Therefore, evidence-based clinical practice guidelines for optimal utilization of imaging are highly recommended. This study identifies our current practice for utilization of lumbar spine imaging in patients with LBP in our outpatient clinic and outcomes based on imaging findings.
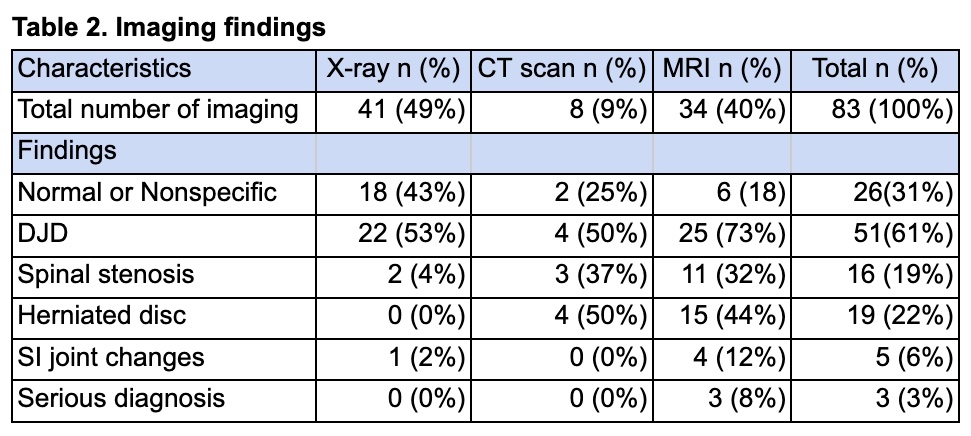
Methods: We used the electronic medical record to generate a patient list, including those 18 years and older who were managed for LBP and referred for lumbar spine imaging between January 1, 2022, and December 31, 2022. Patient demographics, baseline clinical characteristics, and subsequent interventions, such as referrals, counseling, physical therapy, pain management, spinal procedures, opioid prescription, and disability application, were recorded and analyzed using descriptive statistics.
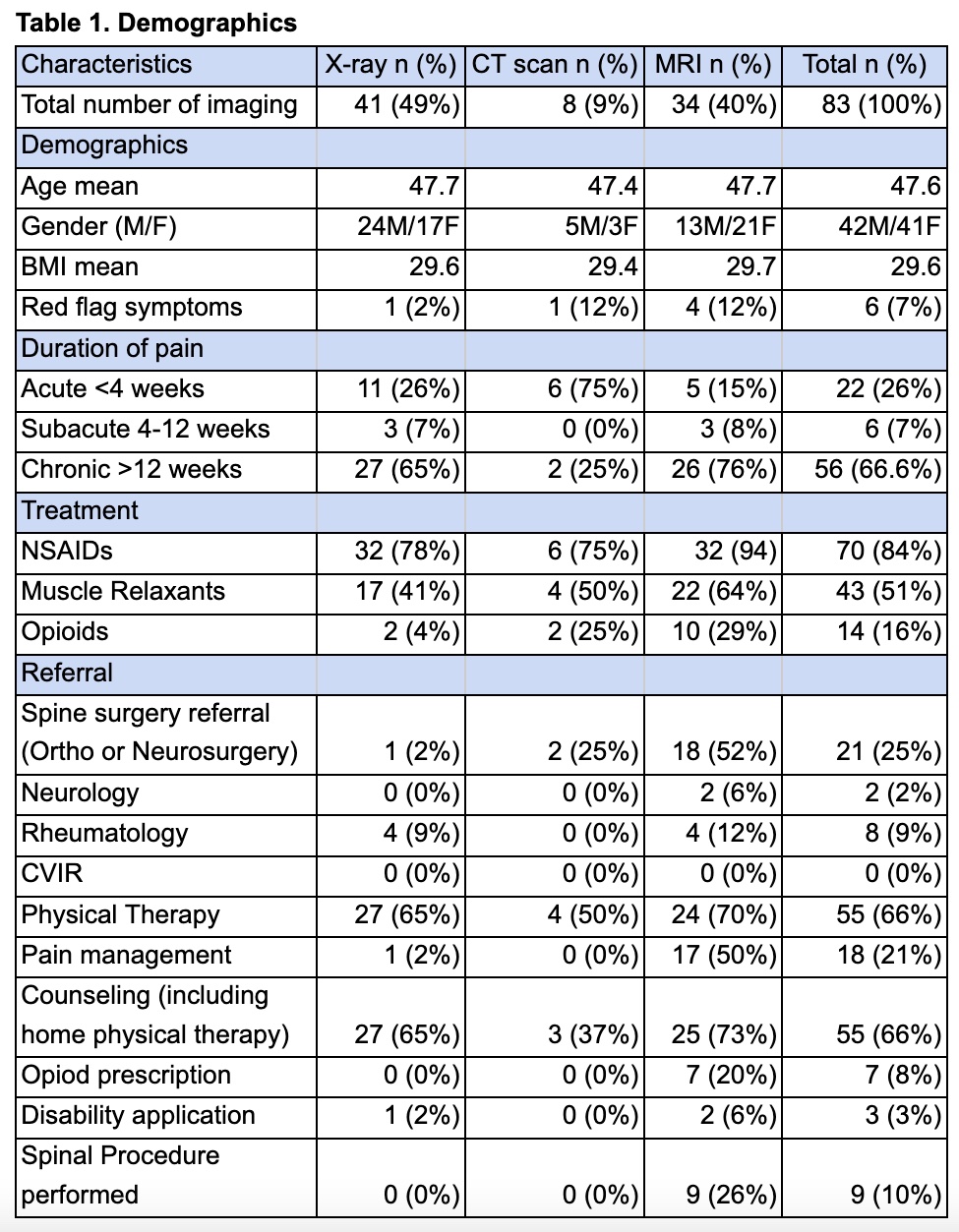
Results: 170 patients were diagnosed with LBP during the study period. Of these, 49% received imaging, with 49% having plain radiography, 9% CT scans, and 40% MRI. 17% of patients had more than one imaging study done, from which 71% had plain radiography followed by MRI. Notably, 82% of those who had plain radiography followed by MRI were done during the chronic course of LBP. Among patients who received imaging, 26% had acute pain, 7% had subacute pain, and 67% had chronic pain. Imaging showed that 43% of the X-ray group had normal or nonspecific results, 73% of the MRI group had degenerative diseases, 44% had herniated discs, and 32% had spinal stenosis. Overall, only 3% of patients had serious diagnoses. Sixty six percent (66%) had lifestyle counseling and referral to physical therapy, 25% of patients were referred to spine specialists, 9% to rheumatologists, and 21% to pain specialists. Half of patients with chronic LBP were treated with muscle relaxants. Only 3% were prescribed opioids and 10% had spinal procedures. Interestingly, 5 patients were referred to rheumatologists for sacroiliac (SI) joint changes.
Conclusion: Majority of LBP in the outpatient setting have an uncomplicated, nonspecific course that require no further diagnostic evaluation. MRI of the lumbar spine is the modality of choice for the majority of patients requiring imaging per ACR appropriateness criteria. Lumbar spine radiographs are of limited utility and are generally only indicated when fracture is a concern. Complete history and careful physical and neurologic examinations are always the cornerstones of LBP management. Our study identifies the current clinical practice for utilization of imaging for patients with LBP among providers in our outpatient clinic. The study recommends further projects to optimize LBP management in our clinic based on evidence-based guidelines.
To cite this abstract in AMA style:
Sereda D, Arcilla C, Arslan K, Goldsmith D. Assessing the Appropriateness of Imaging Modalities in Primary Care for Low Back Pain and Their Impact on Outcomes: A Retrospective Observational Study in a Single Center in Trenton [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/assessing-the-appropriateness-of-imaging-modalities-in-primary-care-for-low-back-pain-and-their-impact-on-outcomes-a-retrospective-observational-study-in-a-single-center-in-trenton/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/assessing-the-appropriateness-of-imaging-modalities-in-primary-care-for-low-back-pain-and-their-impact-on-outcomes-a-retrospective-observational-study-in-a-single-center-in-trenton/