Session Information
Session Type: Poster Session C
Session Time: 8:30AM-10:30AM
Background/Purpose: The goal of rheumatology rotation during internal medicine (IM) residency is to develop competency in work-up and treatment of common rheumatological conditions. IM residents spend less time in rheumatology compared to other subspecialties, necessitating a well-structured curriculum tailored towards resident needs and various clinical settings. In this study, we aimed to identify resident learning needs and preferences during inpatient and outpatient rheumatology rotations to improve the curriculum.
Methods: We distributed surveys to all the current IM residents at the IM Residency Program and rheumatology faculty/fellows in the Section of Rheumatology via email. Rheumatology faculty/fellows were asked to rank 10 rheumatology topics based on the importance. The resident survey assessed confidence in caring for patients with rheumatologic condition in inpatient and outpatient settings on a 10-point Likert scale. Both resident and attending/fellow surveys assessed respondent to rank their preferred learning modality in inpatient and outpatient settings. No validated instruments were available for these purposes; therefore, we created the surveys used in this study.
Results: Out of 13 rheumatology faculty/fellows, 11 (7/4; 84%) completed the survey. Out of 124 residents, 35 (28.2%) including 8 PGY-1, 13 PGY-2, 10 PGY-3, 3 PGY-4 and 1 PGY-5 completed the survey. Among respondents, 37% had rheumatology rotation in medical school and 66% in residency. Four residents (11%) were interested in rheumatology fellowship, and majority (77%) had interest in learning more about rheumatology.
The most important topics to learn during rheumatology rotation per faculty/fellows were knowing when to order and how to interpret autoimmune serologies, followed by musculoskeletal exam and crystalline arthritis (Figure 1). Median confidence level [IQR] among residents for caring for patients with rheumatological conditions was 6 [3.6-7.5] for inpatient and 5 [3.7-6.5] for outpatient settings (10 being very confident). Topics with least reported confidence included joint injections, spondyloarthritis, and other ANA-associated disorders.
Among attendings/fellows, the most preferred outpatient teaching modality was case-based and least preferred was directing trainees to relevant resources. On the inpatient side, directing to relevant resources was the 2nd most preferred modality after bedside teaching (Figure 2). Among residents, the most preferred learning modality was bedside/case-based learning (54-63%) and the least preferred was being directed to resources for self-learning (51-74%) in both settings. Formal lectures were preferred more by residents than attendings/fellows in both settings.
Conclusion: This study showed that average confidence level of residents for most rheumatology topics was moderate (5 out of 10). There was a high degree of concordance between residents and rheumatology faculty/fellows for their preferred education modality in outpatient setting, whereas discordance existed on inpatient setting. Being directed to relevant resources for self-learning was not preferred among residents, while faculty/fellows preferred this option commonly in the inpatient setting.
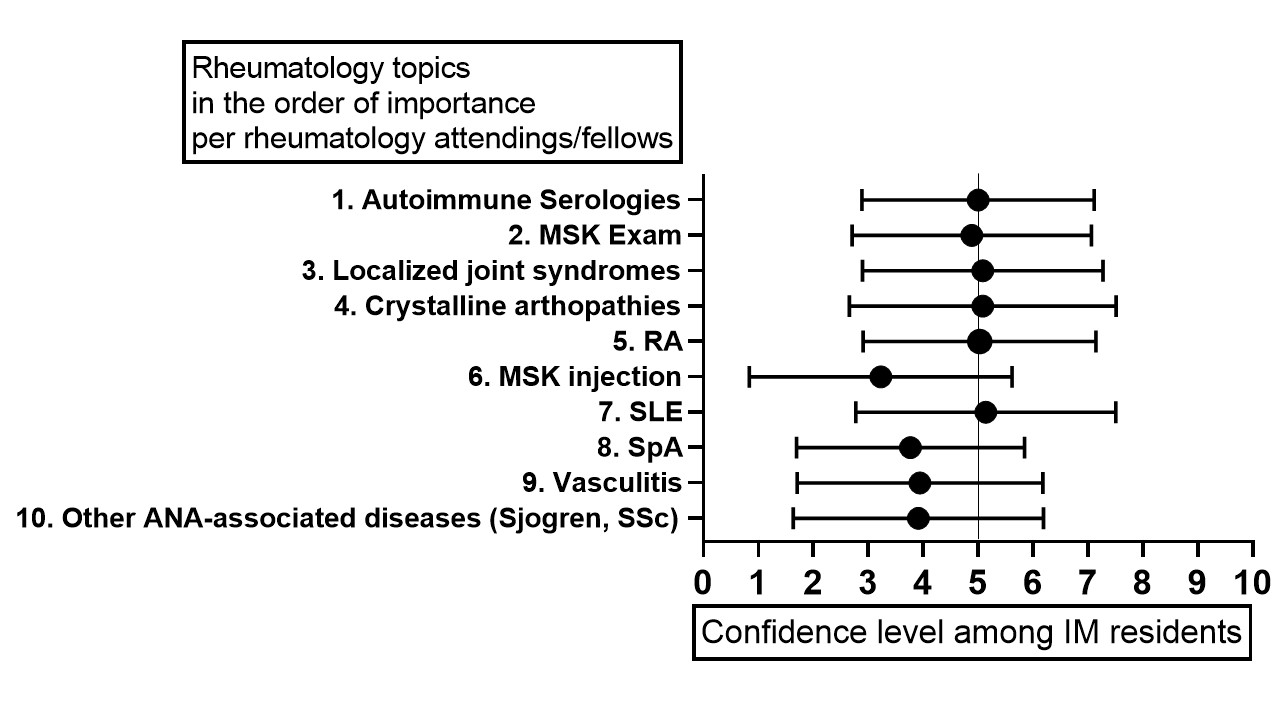 Figure 1. Most important rheumatology topics to learn during rheumatology rotation per rheumatology faculty/fellows and confidence level among residents for each topic [median with IQR]
Figure 1. Most important rheumatology topics to learn during rheumatology rotation per rheumatology faculty/fellows and confidence level among residents for each topic [median with IQR]
 Figure 2. Preferred learning/teaching modalities for rheumatology faculty/fellows and medicine residents in inpatient and outpatient settings
Figure 2. Preferred learning/teaching modalities for rheumatology faculty/fellows and medicine residents in inpatient and outpatient settings
To cite this abstract in AMA style:
He L, Ko K, Quimson L, Leverenz D, Martin S, Saygin D. Assessing Resident Needs and Faculty Perceptions for Rheumatology Curriculum Development [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/assessing-resident-needs-and-faculty-perceptions-for-rheumatology-curriculum-development/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/assessing-resident-needs-and-faculty-perceptions-for-rheumatology-curriculum-development/
