Session Information
Session Type: Poster Session (Monday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Systemic lupus erythematosus (SLE) is a significant risk factor for coronary atherosclerosis, independent of the classic risk factors. Previous studies have found poor acute outcomes in regard to in-hospital mortality and prolonged hospitalizations in SLE patients with acute myocardial infarction. This study aims to examine long term adverse events in lupus patients who have a first time acute coronary syndrome (ACS). We hypothesize that SLE patients with ACS are more likely than age and gender-matched controls to have worse outcomes.
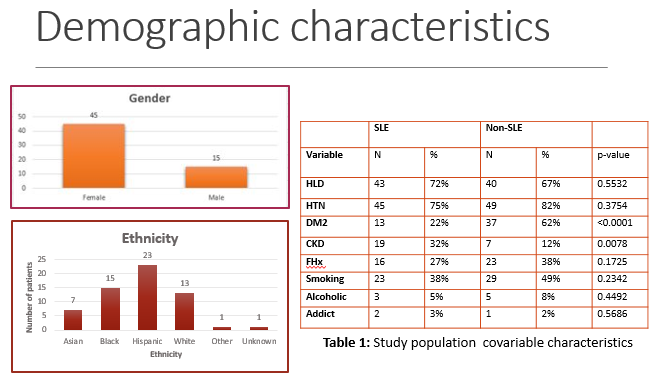
Methods: This is a retrospective study conducted within time frame of 2007-2019 that involved adults above the age of 18. The study comprised of two groups including SLE and non SLE group with 60 patients in each. SLE group consisted of patients diagnosed with SLE who experienced a first time ACS. A second group (non SLE) comprised of randomly selected age, ethnicity, and gender-matched patients with ACS who have no history of SLE. A multivariate analyses was performed to adjust for the confounders. Primary outcome included major adverse clinical events (MACE), including 30-day readmit, 30-day CV readmit, CVA, CHF admission, ACS readmit, and CV death. Secondary outcomes evaluated included LV dysfunction, STEMI, and multivessel CAD.
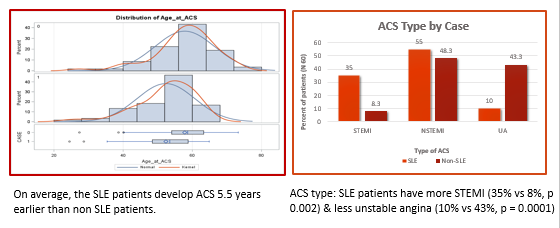
Results: Our results indicated that on average, the SLE patients develop ACS 5.5 years earlier than non SLE patients. There is evidence of more single vessel and more nonobstructive disease in the SLE patients (77% vs 47%, p=0.0003). SLE patients have more STEMI (35% vs 11%, p = 0.002) and less unstable angina (11% vs 42%, p = 0.0001). For MACE, 30-day readmission, 30-day CV readmission, and CV death was more frequent although not statistically significant in patients with SLE. These findings may be statistically significant with bigger sample size that would increase the power of the study or an increased time frame of the study as MACE events of stroke or cardiovascular death may take longer to manifest. Based on propensity score balanced weights, SLE patients have worse LV systolic function and they have less rebound in LVEF during follow up (p value < 0.001).
Conclusion: Based on the results of our study, we conclude that SLE patients develop ACS much earlier than their age, gender, and ethnicity matched non SLE cohort. SLE group has less severe CAD lesions (shown by 1 vessel disease) but more acute events, manifested by STEMI. Inflammatory mediators likely contribute to plaque instability that lead to rupture, thrombosis, and vessel occlusion. Identification of risk factors in SLE patients may enable early and aggressive intervention and risk factor modification. The results of this study show that SLE as an atherogenic risk factor results in worse long-term outcomes for patients with ACS as compared to non-SLE patients including early onset of disease, worse LV function as well as worse 30 day CV readmit. Further directions of this study can implore into whether tighter control of inflammation will reduce the risks of acute ACS events in patients with SLE.
To cite this abstract in AMA style:
Singh P. Assessing Long-term Poor Outcomes in Systemic Lupus Erythematosus Patients with Acute Coronary Syndromes [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/assessing-long-term-poor-outcomes-in-systemic-lupus-erythematosus-patients-with-acute-coronary-syndromes/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/assessing-long-term-poor-outcomes-in-systemic-lupus-erythematosus-patients-with-acute-coronary-syndromes/