Session Information
Session Type: Poster Session A
Session Time: 8:30AM-10:30AM
Background/Purpose: Individuals with anti citrullinated protein antibodies (ACPA) and musculoskeletal complaints are at high risk for developing rheumatoid arthritis (RA) and often seek medical attention due to a symptom burden comparable to that of already diagnosed patients [1] We aimed to investigate the autoimmunity to other autoantibodies, beside ACPA, and study its importance in relation to clinical variables and inflammatory proteins, in risk stratification of predisposed individuals.
Methods: ACPA-positive individuals with musculoskeletal complaints referred from primary care (93%) and other specialist (7%), to a rheumatology clinic were recruited in the Risk-RA Karolinska research program and followed-up for up to 3 years or until arthritis diagnosis (April 2014 and February 2020). In order to investigate early disease mechanisms all individuals lacked both clinical arthritis and subclinical arthritis (measured by ultrasound according to EULAR-OMERACT definitions) in hands, feet and any other symptomatic joints. Blood samples collected at inclusion were analyzed for 14 ACPA specificities along with their arginine counterparts as well as 5 anti-modified protein antibodies (AMPA) against homocitrulline-, acetyl- and lysine- modified filaggrin 307-324 along with acetylated- histone 2B and histone 4 peptides, using custom made peptide array. We further screened for 92 inflammation-associated protein biomarkers (by multiplex immunoassay with Olink extension technology) and HLA-SE (DR low resolution kit). Statistical analysis used univariate and multivariate models with backwards selection and cox regression.
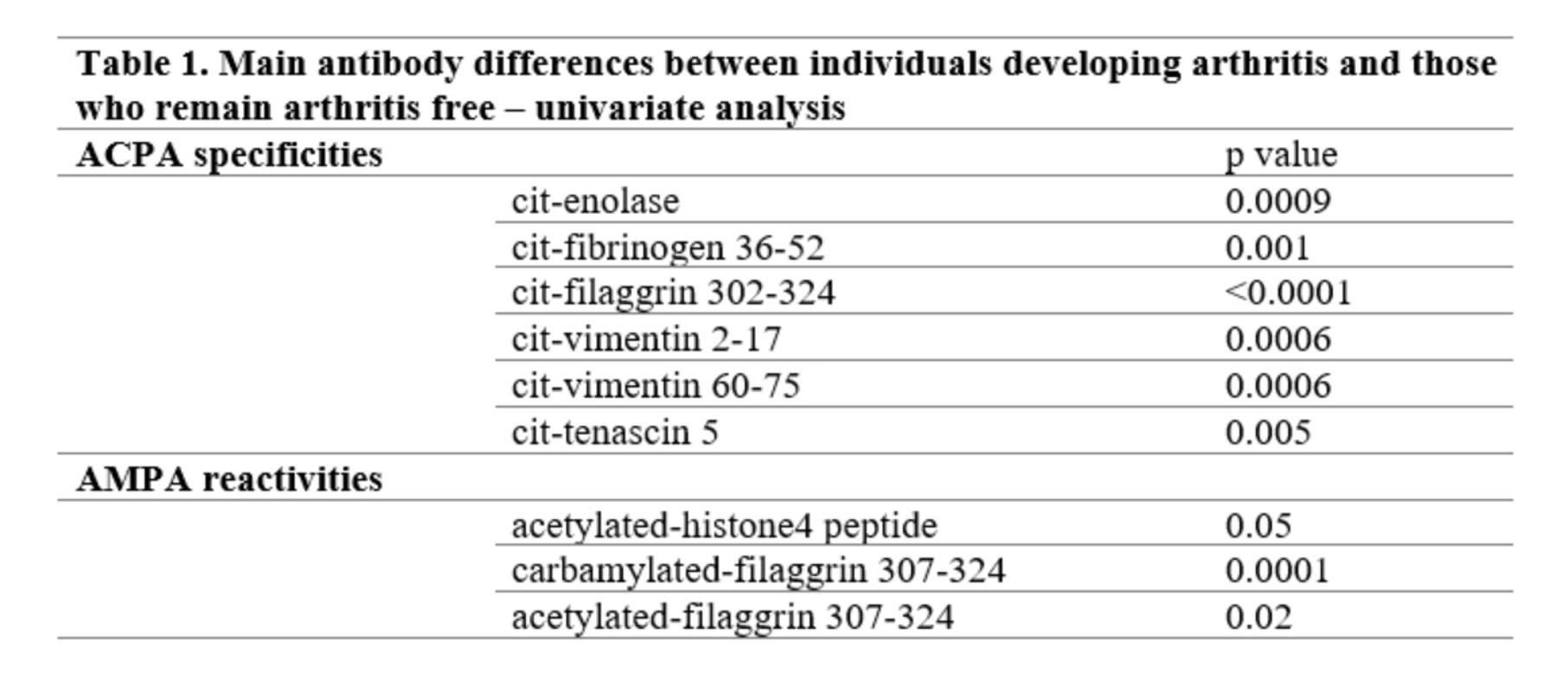
Results: 267 individuals (median age 48 CI: 36-58) were recruited, out of which 210 (78%) were females and with mean presence of 5 ACPA and 1 AMPA reactivities. 79 (30%) developed arthritis within 11 (4-21) months of follow-up compared to 21 (14-28) months median follow-up in those remaining arthritis free. In univariate models, specific ACPAs and AMPAs were associated with progression towards arthritis (Table 1.) Rheumatoid factor positivity (p 0.0003), presence of HLA-SE (p 0.005) and levels of certain inflammatory proteins (CCL20, CXCL6, CXCL9, IL6, IL15, IL17, DNER and TWEAK) associated with arthritis development. In multivariate (backwards selection) cox regression analysis the presence of anti-cit-filaggrin 307-324 (HR 2.1, 95% CI 1.2-3.7, p 0.005), IL6 levels (HR 1.4, 95% CI 1.2-1.7, p< 0.001) and tenosynovitis (HR 2.9, 95% CI 1.7-5.0, p < 0.001) remained significant predictors for arthritis onset. All other types of AMPA for filaggrin lost significance.
Conclusion: Risk-RA phase is characterized by several types of ACPAs and AMPAs, however anti-cit-filaggrin and ACPA reactivities show the strongest risk for progression to arthritis along with inflammatory proteins and ultrasound-detected tenosynovitis. The biological mechanisms need to be further explored in detail.
References:
[1] Studenic P., et al. Symptoms characteristics of seropositive individuals at-risk for developing rheumatoid arthritis are versatile and comparable to those in people with early rheumatoid arthritis, accepted abstract EULAR 2021
To cite this abstract in AMA style:
Circiumaru A, Kisten Y, Hansson M, Wähämaa H, Sun M, Joshua V, Rezaei H, Af Klint E, Antovic A, Catrina A, Haj Hensvold A. Arthritis Progression in at Risk Individuals Is Associated with ACPAs Not AMPAs [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/arthritis-progression-in-at-risk-individuals-is-associated-with-acpas-not-ampas/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/arthritis-progression-in-at-risk-individuals-is-associated-with-acpas-not-ampas/