Session Information
Session Type: Poster Session (Tuesday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Patients with rheumatoid arthritis (RA) are predisposed to impaired cardiac function and heart failure (HF). While the pathophysiology has not been fully elucidated yet, inflammation is suspected to play an important role. However, the impact of disease-modifying antirheumatic drugs on cardiac dysfunction in RA remains controversial. Although anti-inflammatory drugs might have protective effects, some of them, i.e. tumour necrosis factor inhibitors (anti-TNF), might also negatively influence cardiac function. Serum N-terminal pro-brain natriuretic peptide (s-NT-proBNP) is used as a biomarker of cardiac function, and levels ≤125 ng/L with high probability exclude HF1.
To examine effects of methotrexate (MTX) and anti-TNF regimens on s-NT-proBNP in patients with active RA, and to assess associations between s-NT-proBNP and endothelial function (EndoF).
Methods: From the observational PSARA study, we examined 64 RA patients starting with MTX monotherapy (n=34) or anti-TNF with MTX co-medication (n=30) due to active disease. All patients starting with anti-TNF regimens had been previously unsuccessfully treated with MTX. s-NT-proBNP (ELISA), EndoF (measured by finger plethysmography), and other laboratory and clinical parameters were evaluated at baseline and after 6 weeks and 6 months of treatment.
Results: Median age was 57 years (range 28-79), and 73% were women. 17 (27%) patients had CVD (history of angina, MI, heart surgery, PTA, cerebrovascular disease, thromboembolism, aortic aneurysm, peripheral artery disease). None of the patients had known/symptomatic HF. There were no statistically significant differences between s-NT-proBNP levels at baseline (median 2241 ng/L [IQR 9002]) and after 6 weeks (median 2300 ng/L, [IQR 8960]) and 6 months (median 2358 ng/L [IQR 7772]) of antirheumatic therapy (p=0.992 and p=0.528, respectively). There were no significant differences in the effects of MTX monotherapy and anti-TNF regimens on s-NT-proBNP levels (pbaseline-6weeks=0.779; pbaseline-6months=0.421). At baseline, 57 (89%) patients had s-NT-proBNP >125 ng/L, and 44 (69%) had high s-NT-proBNP levels (s-NT-proBNP >450 ng/L in patients < 50 years old and >900 ng/L in patients ≥50 years old), and these frequencies did not significantly change with antirheumatic treatment. s-NT-proBNP was not related to EndoF.
Conclusion: A large proportion of RA patients without known HF had elevated s-NT-proBNP levels, which might indicate subclinical impairment of cardiac function. s-NT-proBNP levels were not influenced by six-month MTX and/or anti-TNF treatment. Thus, in contrast to some previous studies, our data does not support the notion that anti-inflammatory treatment protects against HF, and that anti-TNF treatment has negative effect on cardiac function in RA. Nevertheless, definitive conclusions cannot be drawn by our study, e.g. due to limitations of s-NT-proBNP as surrogate marker of HF. Cardiac function in terms of s-NT-proBNP levels was not related to EndoF.
Reference
Ponikowski P et al. European journal of heart failure. 2016;18:891-975.
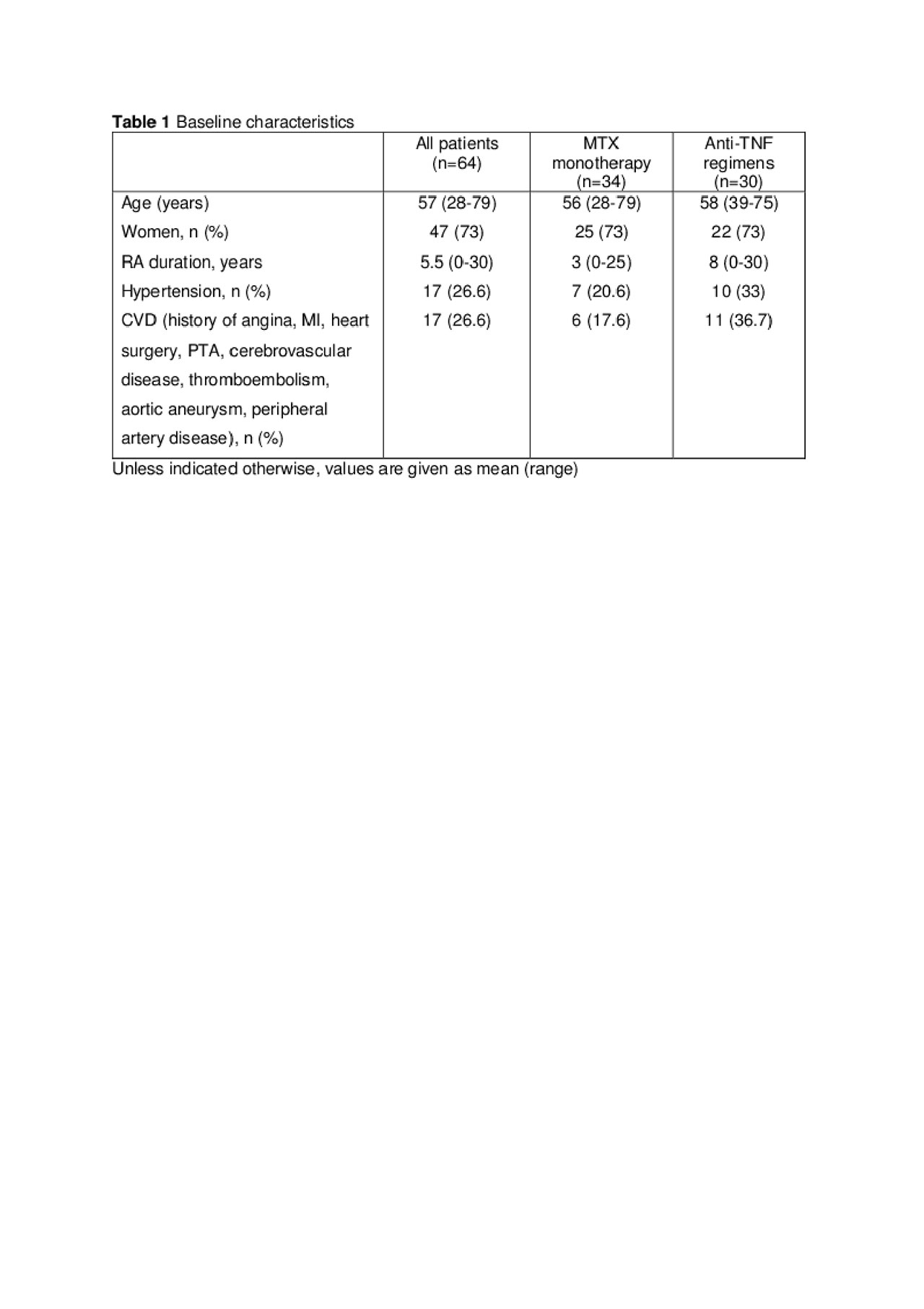
Abstract NT-pro-BNP – Table 1 Baseline characteristics pdf
To cite this abstract in AMA style:
Nguyen T, Deyab G, Fagerland M, Agewall S, Eilertsen G, Feinberg M, Mikkelsen K, Førre �, Hollan I. Antirheumatic Therapy Is Not Associated with Changes in Circulating N-terminal Pro-brain Natriuretic Peptide Levels in Patients with Active Rheumatoid Arthritis [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/antirheumatic-therapy-is-not-associated-with-changes-in-circulating-n-terminal-pro-brain-natriuretic-peptide-levels-in-patients-with-active-rheumatoid-arthritis/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/antirheumatic-therapy-is-not-associated-with-changes-in-circulating-n-terminal-pro-brain-natriuretic-peptide-levels-in-patients-with-active-rheumatoid-arthritis/
