Session Information
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Thrombocytopenia (TP) is a common hematologic abnormality in systemic lupus erythematosus (SLE). Severe thrombocytopenia is correlated with disease activity and a worse prognosis of SLE associated thrombocytopenia (SLE-TP). Antiphospholipid antibodies (aPLs)have been proven to cause low platelet count through various mechanisms. However, the impact of aPLs on SLE-TP remains a matter of debate. In this multicenter prospective study, we aim to investigate the role of aPLs on disease severity and prognosis of SLE-TP.
Methods: All SLE patients fulfilled the 2019 the American College of Rheumatology (ACR) / the European League Against Rheumatism(EUALR) classification criteria for SLE. Antiphospholipid syndrome (APS) was diagnosed according to the revised 2006 Sapporo APS classification criteria. TP was defined as a platelet count<100×109/L, and patients with TP due to other causes were excluded. aPLs were tested following international guidelines (anticardiolipin, anti-β2 glycoprotein I antibodies and lupus anticoagulant). Demographic characteristics, platelet count, clinical manifestations, disease activity, and autoantibody profiles were collected at baseline. Severity of thrombocytopenia was categorized into mild, moderate, and severe group. Relapse was defined as the loss of remission. Bone marrow punctures indicated impairment of megakaryocyte maturation.
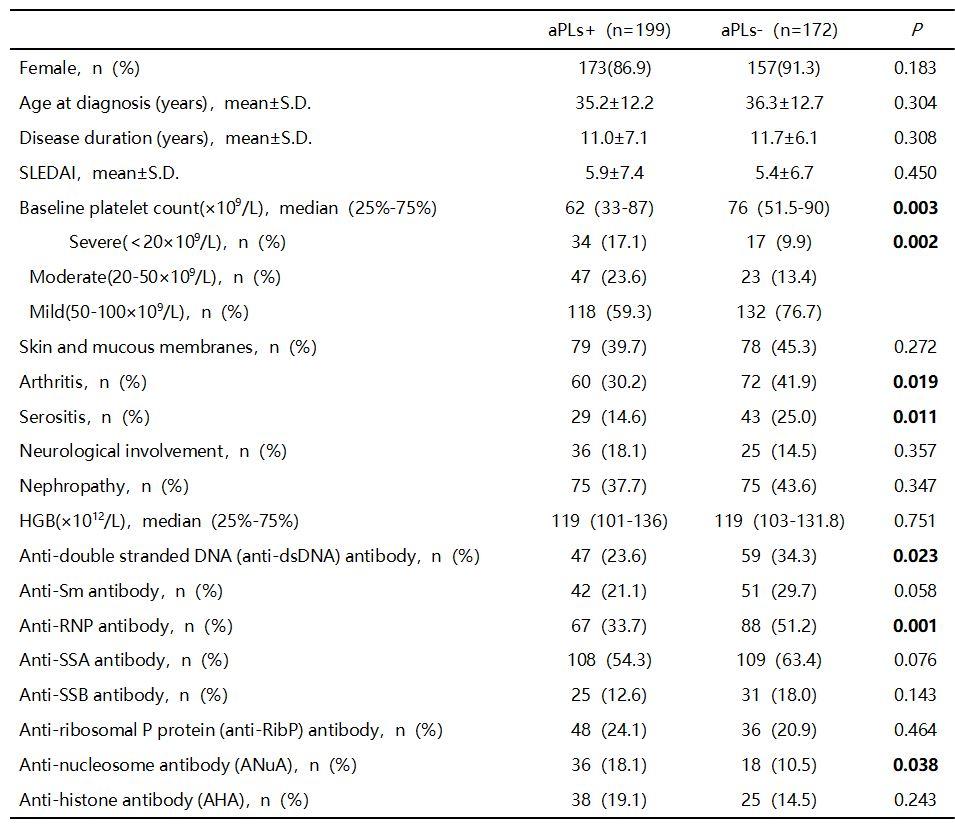
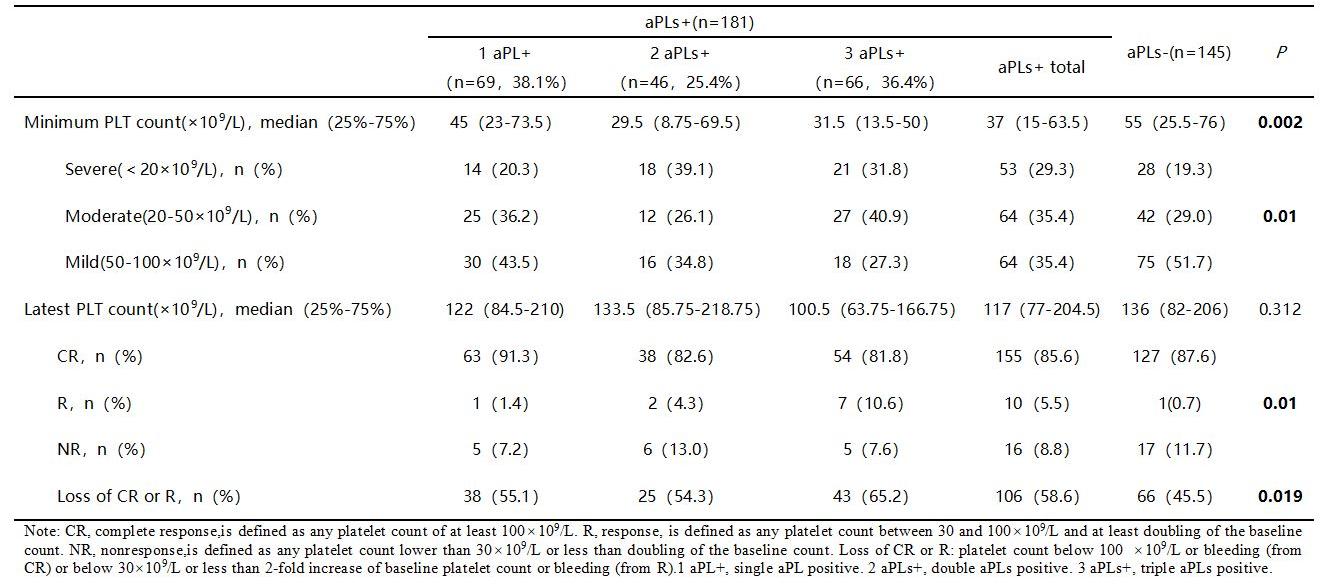
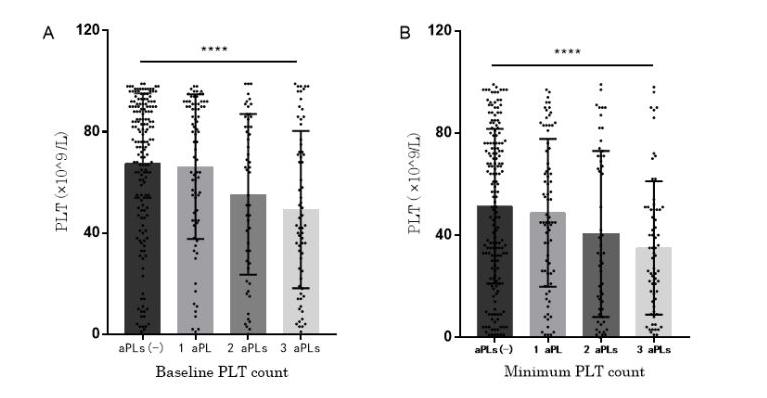
Results: A total of 371 SLE-TP patients with complete follow-up data were enrolled, out of which 199 (53.6%) were aPLs positive and 48 (24.1%) were complicated with APS. Baseline comparison showed that SLE-TP with aPLs had lower baseline platelet counts (62.0×109/L vs. 76.0×109/L, P=0.003), and a higher proportion of moderate to severe cases (17.1% vs. 9.9%; 23.6% vs. 13.4%, P=0.002). SLE-TP patients with aPLs had lower platelet counts at their lowest point (37.0 × 109/L vs. 55.0 × 109/L, P=0.002).In addition, the increasing number of aPLs types was associated with the decrease of baseline and minimum values of platelets (P < 0.001; P=0.001). SLE-TP carrying aPLs had a lower prevalence of arthritis (39.7% vs. 45.3%, P=0.019) and serositis (14.6% vs. 25.0%, P=0.011).Among aPLs carriers, there was a higher positivity rate for ANuA (18.1% vs. 10.5%, P=0.038), whereas it was lower for anti-RNP antibody (33.7% vs. 51.2%, P=0.001). During a median 5.47-year follow-up of 326 SLE-TP patients with complete treatment data (181 aPLspositive, 55.5%), SLE-TP carrying aPLs hada higher relapse rate(58.6% vs.45.5%, P=0.019) and lower complete response (CR) rate (85.6% vs.87.6%). Furthermore, the analysis of 61 SLE-TP with qualified bone marrow reports found that there was no significant difference in ratio of granulocytes to red blood cells (G/E), the total number of megakaryocyte and categories (granulosa, naked nuclear, and plate producing cells).
Conclusion: SLE-TP with positive aPLs had more severe disease condition and a higher recurrence rate, which suggests that we should implement more proactive management strategies and maintain vigilance towards relapse in SLE-TP patients with positive aPLs.
To cite this abstract in AMA style:
Birru Talabi M, Bermas B, Blanco I, Blazer A, Clowse M, Edens C, Pierce L, Wright C, Ramsey-Goldman R. Antiphospholipid Antibodies as Potential Predictors of Disease Severity and Poor Prognosis in Systemic Lupus Erythematosus Associated Thrombocytopeinia [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/antiphospholipid-antibodies-as-potential-predictors-of-disease-severity-and-poor-prognosis-in-systemic-lupus-erythematosus-associated-thrombocytopeinia/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/antiphospholipid-antibodies-as-potential-predictors-of-disease-severity-and-poor-prognosis-in-systemic-lupus-erythematosus-associated-thrombocytopeinia/