Session Information
Date: Tuesday, October 28, 2025
Title: (2377–2436) Systemic Lupus Erythematosus – Diagnosis, Manifestations, & Outcomes Poster III
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: It has been reported that the presence of positive ANA in patients treated with TNF inhibitors (TNFi) could be associated with the development of new clinical symptoms of SLE. The aim of this study is to review the prevalence of positive ANA titers by immunofluorescence assay (IF-ANA) in patients with psoriasis (PSO) and PsA, as well as the associated risk of developing clinical symptoms of SLE after treatment with TNFi.
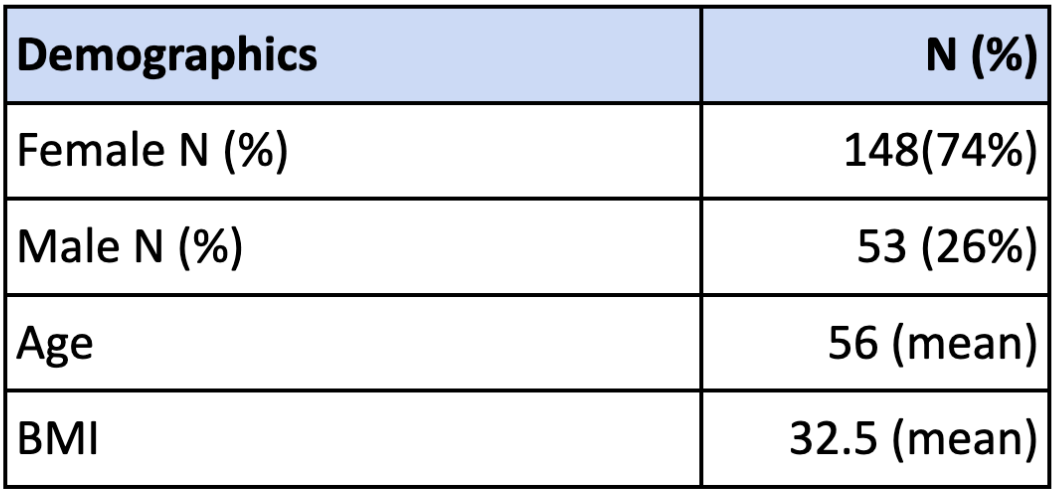
Methods: The study utilized the electronic medical record system to generate a list of patients who were diagnosed with PSO or PsA between 2014 and 2024. From this list, patients with a positive IF-ANA titer ( >1:80) who were treated with TNFi were selected. A detailed chart review was then performed to identify those who developed drug-induced SLE-like symptoms following TNFi therapy.Descriptive statistics were used to analyze demographic data (Table 1), and the Chi-square and Fisher’s exact tests were employed to assess relationships between groups and binary outcomes.
Results: Over the ten-year period, 9,273 individuals were diagnosed with PSO or PsA. Among them, 1,171 patients were tested for IF-ANA, of whom 518 tested positive and 653 tested negative. Among the IF-ANA positive patients, 187 were treated with TNFi (Table 2). Some of these patients received more than one TNFi agent during the course of treatment. Notably, 20 patients developed IF-ANA positivity only after initiating TNFi therapy.Based on clinical visit notes, 42 patients were suspected of developing drug-induced lupus. Among them, 7 reported worsening joint pain and fatigue, 17 developed worsening or new skin rashes, 3 patients had a significant increase in IF-ANA titers ( >6,000), 2 patients developed new anti-dsDNA antibodies, and 1 patient developed anti-histone antibodies. Additional findings included transaminitis in 3 patients, a demyelinating disorder in 1 patient, and paresthesia in 4 patients. Four patients developed other symptoms, including one case each of pericarditis, allergic reaction, diverticular rupture, and pancytopenia (Table 3). Furthermore, 69 IF-ANA–positive patients did not respond to TNFi treatment.
Conclusion: The association between TNFi use and SLE-like symptoms remains a clinical concern. TNFi can elevate ANA titers in ANA-positive patients and may induce new ANA positivity in ANA- negative individuals (2). TNFi have been linked to drug-induced lupus, presenting with arthralgias, rashes, and serositis (1). Diagnosis typically requires symptom onset after TNFi initiation, one positive autoantibody (e.g., ANA or anti-dsDNA), and one non-serologic criterion such as rash (4). In our review, 20 of 187 patients developed new ANA positivity. Although ANA and anti-dsDNA positivity were low, SLE-like symptoms were statistically significant, with joint pain and rash being the most common. The 72% of affected patients were on adalimumab. Prior studies suggest higher lupus risk with adalimumab and infliximab, though all TNFi can induce ANA (1). Some patients may tolerate a different TNFi without recurrence (5). Proposed mechanisms include reduced CD44 expression, infection-induced autoantibodies, and a cytokine shift toward Th2 responses (3), possibly explaining variable risk across TNFi agents.
.jpg) Table 2. Percentage of patients treated with different TNFi agents.
Table 2. Percentage of patients treated with different TNFi agents.
.jpg) Table 3. Chi-square statistics.
Table 3. Chi-square statistics.
To cite this abstract in AMA style:
Sereda D, Leechalad L, Perl A. Antinuclear Antibody Positivity in Patients with Psoriasis and Psoriatic Arthritis and the Risk of Developing Clinical Symptoms of SLE Following TNF Inhibitor Therapy [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/antinuclear-antibody-positivity-in-patients-with-psoriasis-and-psoriatic-arthritis-and-the-risk-of-developing-clinical-symptoms-of-sle-following-tnf-inhibitor-therapy/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/antinuclear-antibody-positivity-in-patients-with-psoriasis-and-psoriatic-arthritis-and-the-risk-of-developing-clinical-symptoms-of-sle-following-tnf-inhibitor-therapy/