Session Information
Date: Monday, October 27, 2025
Title: (1147–1190) Miscellaneous Rheumatic & Inflammatory Diseases Poster II
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: There is increasing evidence of the association between interstitial lung disease (ILD) and ANCA positivity without other manifestations of systemic vasculitis. The prognosis of these patients remains uncertain, particularly in terms of their risk of progressing to systemic vasculitis, and the appropriate treatment approach is yet to be established. Our objective was to investigate the clinical characteristics, outcomes, and response to treatment in a cohort of patients with ANCA-positivity with isolated ILD (ANCA-ILD).
Methods: Retrospective study of patients diagnosed with ANCA-ILD at a Pulmonary Interstitial Unit in a tertiary university hospital. Diagnosis was made in cases of ANCA positivity and isolated pulmonary fibrosis, with no apparent development of systemic manifestations over a minimum period of 9 months. Patients were monitored from the date of ANCA-ILD diagnosis until death or the last follow-up
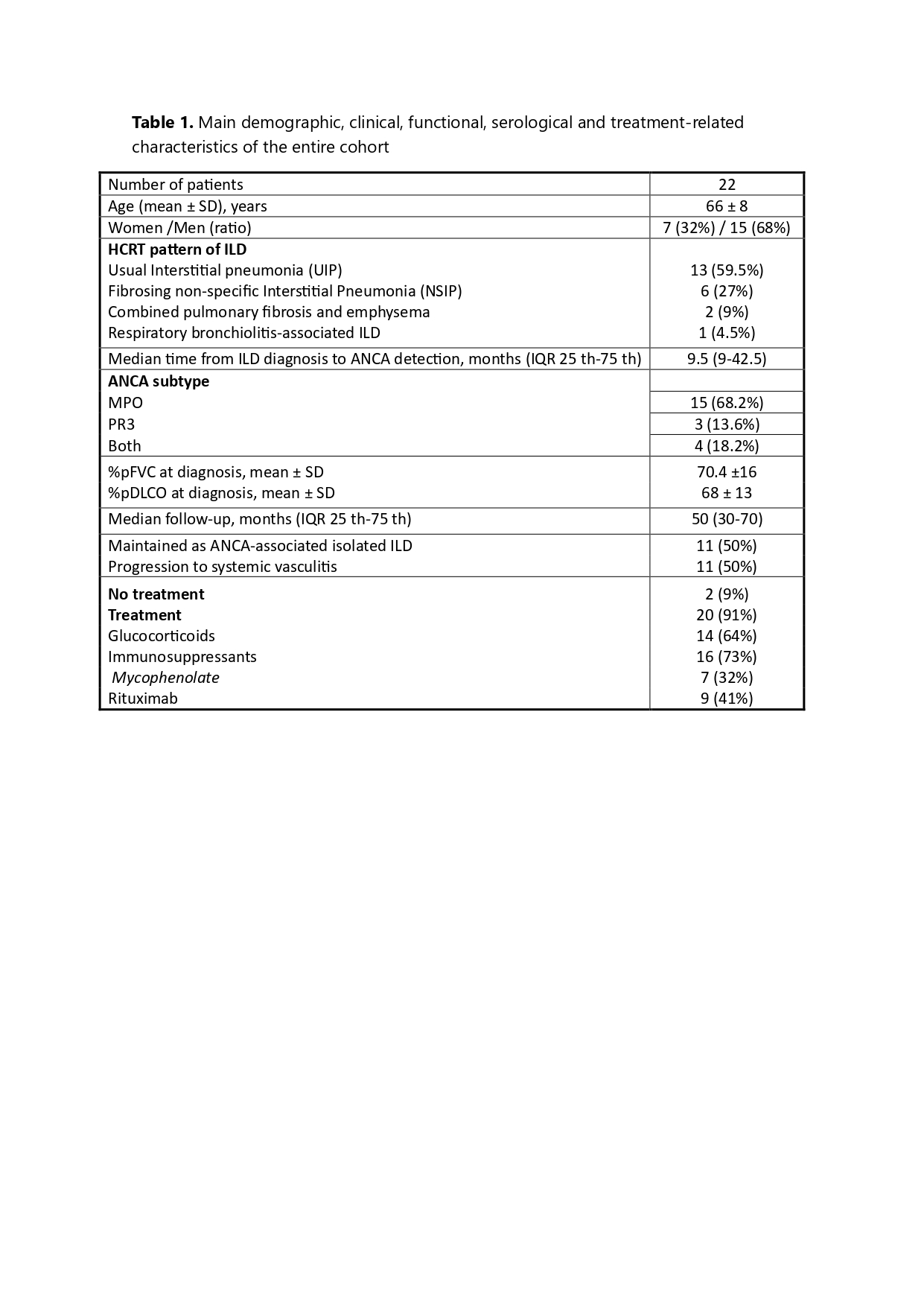
Results: We identified 22 patients (15 men) with a mean age at diagnosis of 66 ± 8 years. Their main clinical features and laboratory data are summarized in Table 1. The predominant radiological pattern was usual interstitial pneumonia (UIP), observed in 59.5% of cases. This was followed by fibrosing non specific interstitial pneumonia (NSIP) in 27% of cases, combined pulmonary fibrosis and emphysema in 9%, and respiratory bronchiolitis-associated interstitial lung disease in 4.5%. The median time from ILD diagnosis to ANCA detection spanned 9.5 months, with a range of 9 to 42.5 months. The identified ANCA subtypes were MPO in 68.2% of cases, PR3 in 13.6%, and both subtypes in 18.2%. Initial treatment involved glucocorticoids in 64% of cases and antifibrotic therapy in 59%. After a median follow-up of 54 months (IQR 25th-75th 15 – 90.5), 50% of the patients had developed clinical signs of PAM or GPA-type vasculitis after a median follow-up of 50 months post-ANCA detection (IQR 25th -75th 30-70). These patients received treatment with rituximab (73%) or MMF (27%). None of the patients died, but three developed chronic respiratory failure and became candidates for lung transplantation. Among the remaining 11 patients, who continued with a diagnosis of ANCA-associated isolated ILD and received treatment with low-dose glucocorticoids and antifibrotic therapy (72.7%), 45.5% showed pulmonary progression and required additional immunosuppressive treatment (MMF and, in one case, rituximab). Furthermore, 27.3% developed chronic respiratory failure, and there was an 18.1% mortality rate. No predictive risk factors for the progression to systemic vasculitis were identified. ANCA-MPO levels were notably higher in patients with generalized vasculitis (153±93 versus 76±48; p=0.346). Of the patients with ANCA-PR3, only 57.1% progressed to systemic vasculitis.
Conclusion: Approximately three-quarters of patients initially diagnosed with ANCA-positive isolated ILD showed pulmonary progression, and approximately half eventually developed symptoms of systemic vasculitis during the follow-up period. The use of antifibrotics and immunosuppressants seemed to slow the progression of lung disease
To cite this abstract in AMA style:
Narváez J, Maymó-Paituvi P, Vicens Zygmunt V, Bermudo G, Aguilar-Coll M, Roig Kim M, De Daniel Bisbe L, Nolla J, Molina-Molina M. Antineutrophil cytoplasmic antibody-associated isolated interstitial lung disease [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/antineutrophil-cytoplasmic-antibody-associated-isolated-interstitial-lung-disease/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/antineutrophil-cytoplasmic-antibody-associated-isolated-interstitial-lung-disease/