Session Information
Session Type: Poster Session A
Session Time: 1:00PM-3:00PM
Background/Purpose: Interstitial lung disease (ILD) is a major cause of morbidity and mortality in patients with idiopathic inflammatory myositis (IIM). Anti-SSa/SSb and Ro52 are frequently reported in myositis. We have previously reported an association between presence of SSa/SSb antibodies and interstitial lung disease (ILD). The aim of this analysis was to evaluate the prognostic utility of anti-SSa/SSb and Ro52 in predicting severity and progression of ILD in IIM patients.
Methods: This is a follow up analysis of the Northwell Myositis cohort incepted 1/1/2007- 4/6/2018 ensuing through 6/1/2022. All patients met 2017 EULAR/ACR classification criteria for IIM and had anti-SSa/SSb serologies available. Anti-SSb was only found in association with anti-SSa in this cohort and was analyzed as a single group.Diagnosis of ILD was defined by presence of NSIP, COP/BOOP, UIP, and unspecified patterns on CT chest and confirmed by chart review. PFTs were analyzed at baseline and longitudinally over a 48-month period. Descriptive statistics, ANOVA and repeated measures ANOVA (non-parametric) were used for statistical analysis.
Results: Of 94 patients in the cohort, 36.2% (34/94) had a diagnosis of ILD, 22 patients had at least 2 PFTs and were included in follow-up analysis.
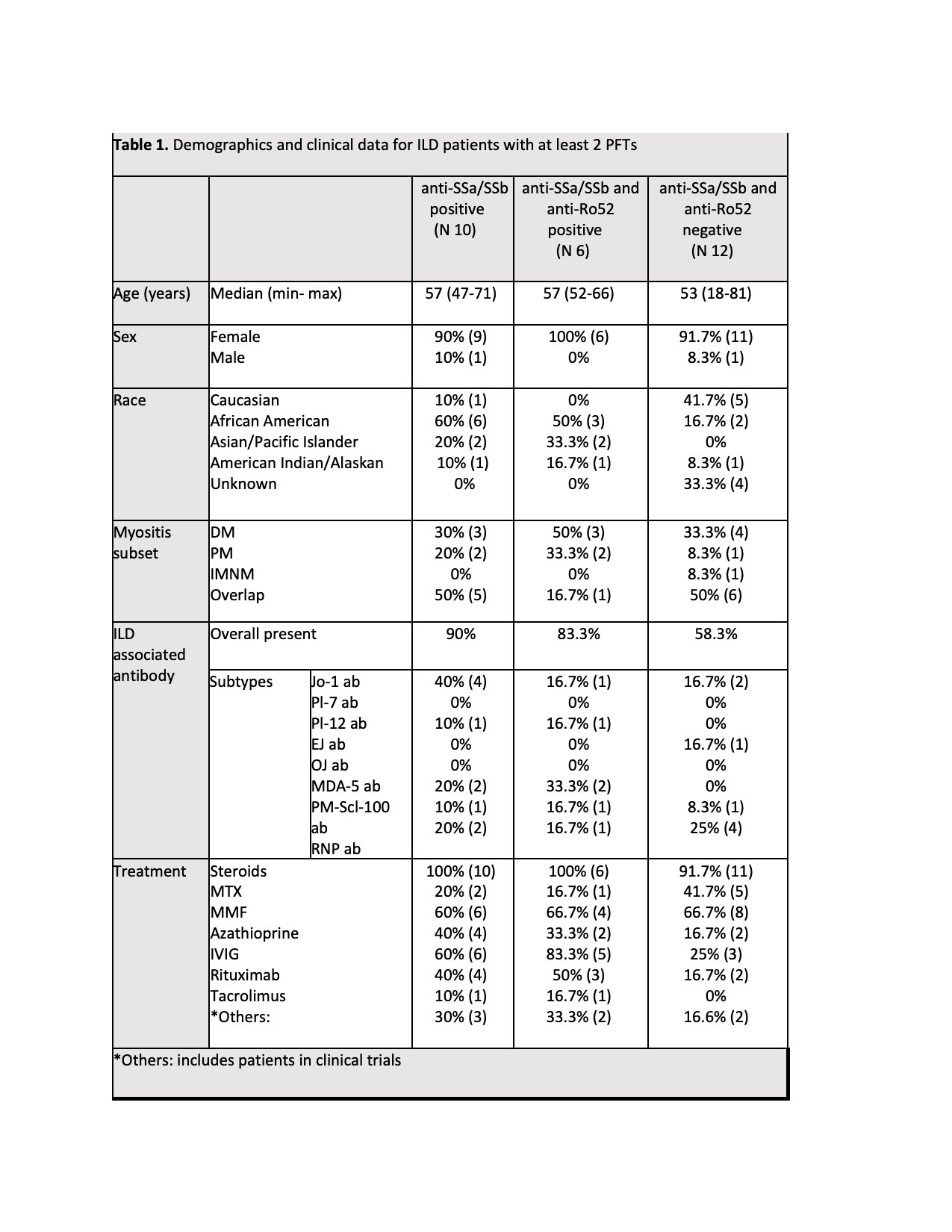
45.5% (10/22) patients were anti-SSa/SSb positive, of which, 27.3% (6/22) were double positive, 54.5% (12/22) patients were negative for anti-SSa/SSb and anti-Ro52. Demographics, clinical characteristics, and medications are presented in Table 1.
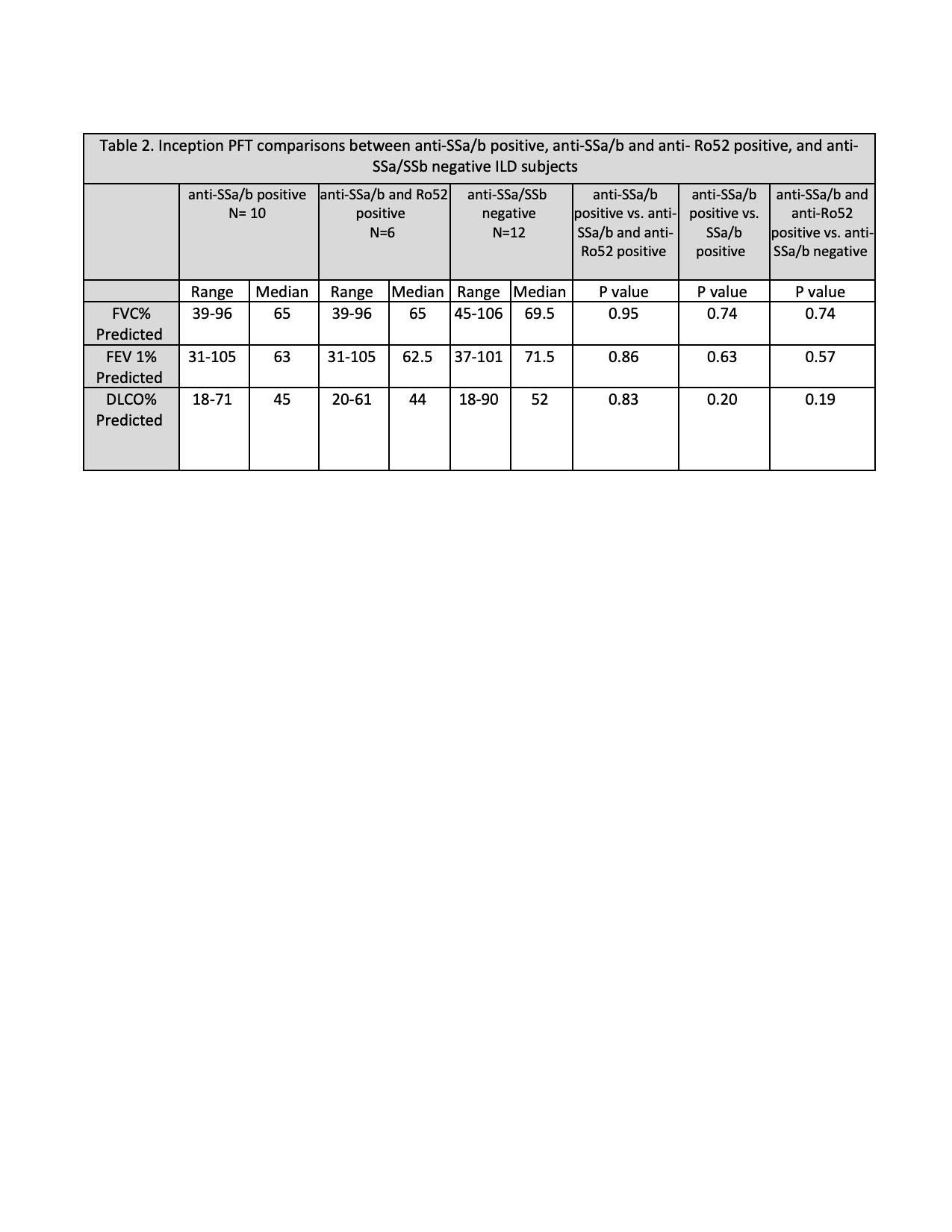
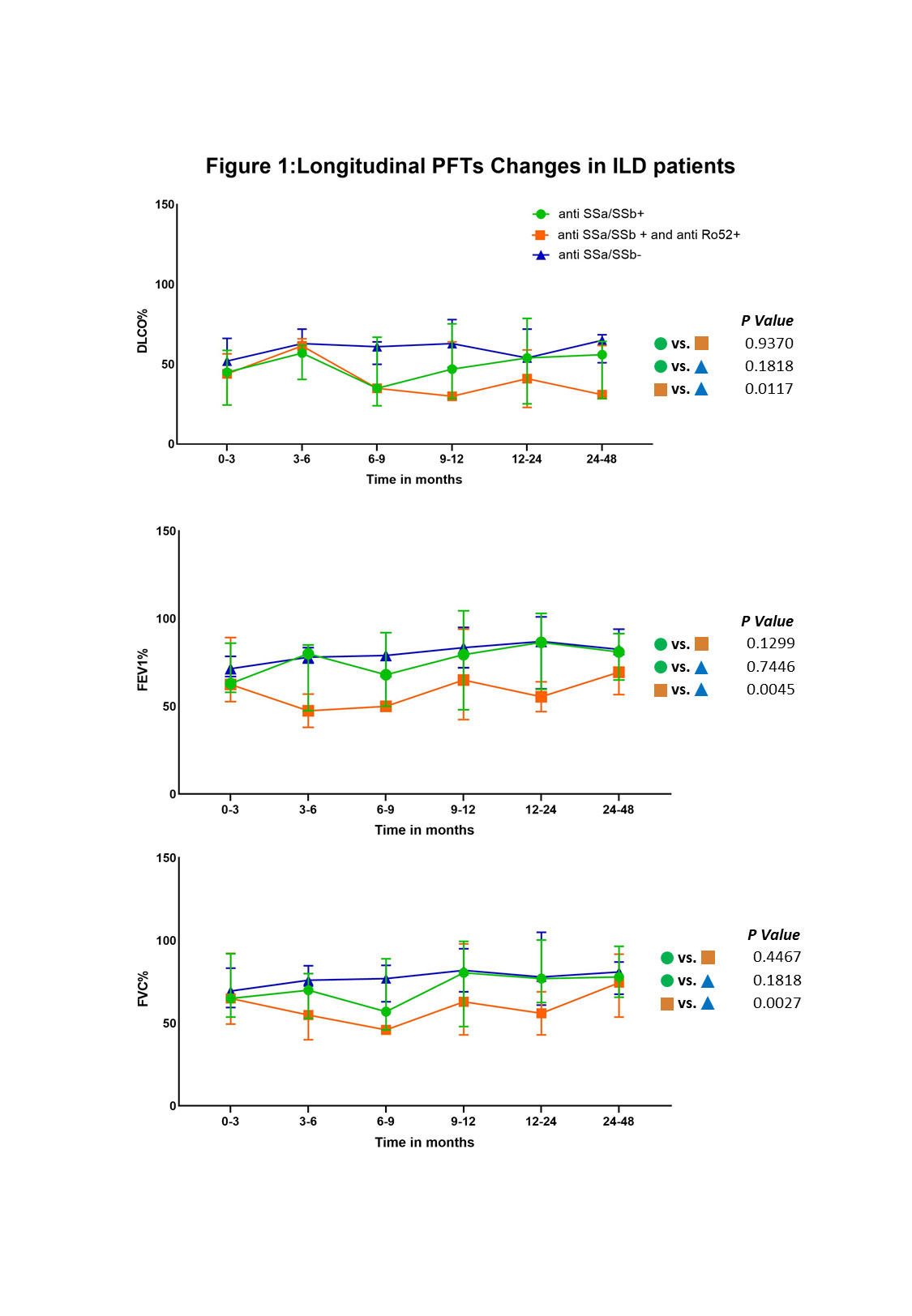
PFT parameters (FVC, FEV1 and DLCO) were similar across all 3 groups at the time of inception as shown in Table 2. During the 48-month follow-up, FVC, FEV1 and DLCO remained stable over time in the anti-SSa/SSB negative group (n=39). While there were fluctuations in the FVC, FEV1 and DLCO in both anti-SSa/SSb positive (n=37) and the double positive groups (n=19), a statistically significant decline was observed in the double positive group when compared to the anti-SSa negative group (FVC, p = 0.0117; FEV1, p = 0.0045; and DLCO p = 0.0027). This difference was not observed between the anti-SSa/SSB positive and the double positive groups nor between the anti-SSa/SSb positive and negative groups. PFT change time over time in each group is shown on Figure 1.
Conclusion: In patients with diagnosis of ILD, the presence or absence of anti-SSa/SSb and anti-Ro52 did not affect baseline PFT parameters. IIM associated ILD patients, irrespective of anti-SSA/SSB positivity, tend to maintain their pulmonary function over time. However, patients who are anti-Ro52 positive are more likely to decline despite aggressive therapy. This further supports that presence of Ro52 antibodies is a negative prognostic marker for ILD in patients with IIM.
To cite this abstract in AMA style:
Ahmed A, Narain S, Ilic I, Hu C, Bhatti J, Marder G. Anti-SSa/SSb and Ro52 Status and Pulmonary Function Tests in Patients with Interstitial Lung Disease and Idiopathic Inflammatory Myopathies [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/anti-ssa-ssb-and-ro52-status-and-pulmonary-function-tests-in-patients-with-interstitial-lung-disease-and-idiopathic-inflammatory-myopathies/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/anti-ssa-ssb-and-ro52-status-and-pulmonary-function-tests-in-patients-with-interstitial-lung-disease-and-idiopathic-inflammatory-myopathies/