Session Information
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Pneumologists do not routinely include screening for anti-neutrophil cytoplasmic antibodies (ANCA) in the evaluation of interstitial pneumonia (IP). Indeed, antibodies against myeloperoxidase (anti-MPO) and proteinase 3 (anti-PR3) are not encompassed in the classification of IP with Autoimmune Features (IPAF), However, anti-MPO antibodies have been reported in subjects with ILD or idiopathic bronchiectasis (percentage ranging from 7 to 23%), but only a few studies describe their clinical evolution. The aim of this study was to evaluate the prevalence of anti-neutrophil cytoplasmic antibodies (ANCA), anti-MPO antibodies and anti- proteinase-3 (ant-PR3) antibodies in patients with Idiopathic pulmonary fibrosis (IPF) and IPAF in a pneumologist setting.
Methods: We retrospectively collected clinical charts of patients referred to a Pneumology Clinic specialized in IP, who received a diagnosis of IPF/IPAF from 31 March 2018 to 1 April 2023. We re-tested all patients for IPAF-associated autoantibodies (ANA, ENA, anti-CCP, RF) and ANCA, anti-MPO or ant-PR3. Descriptive statistics were performed for demographic and disease characteristics. Analysis of outcome predictors was performed by logistic multiple logistic regression. To identify the clinical subset of IP patients with baseline features at higher odds to progress to systemic vasculitis, unsupervised clustering with K-means fitted with all baseline covariates was performed.
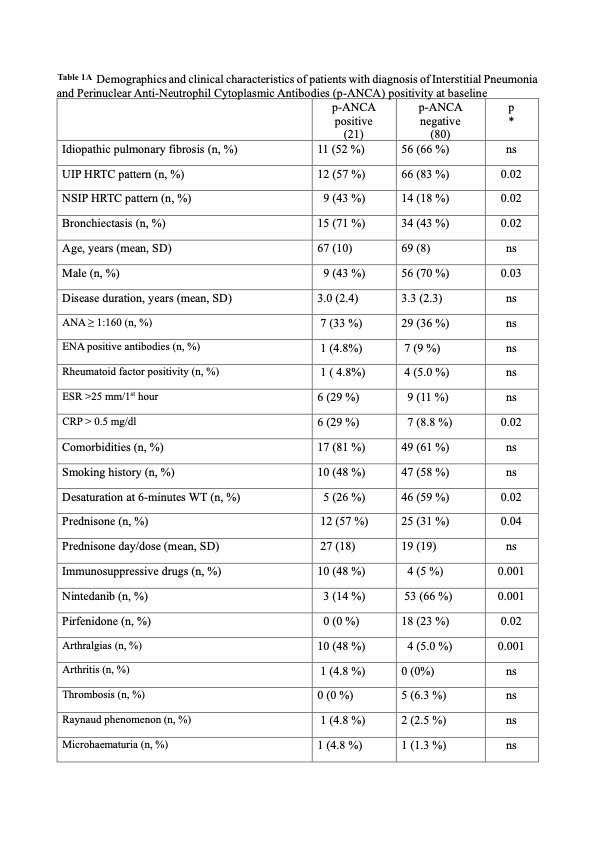
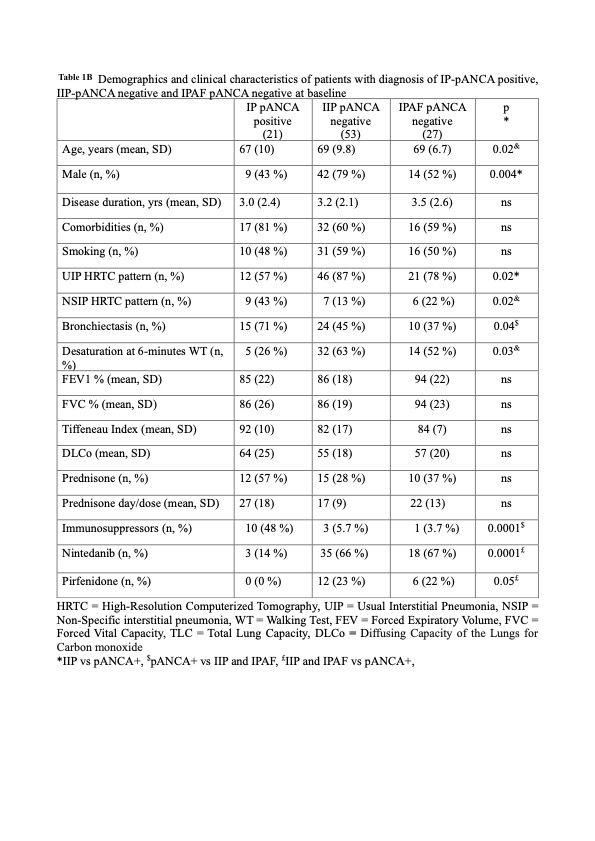
Results: Our cohort was made of 101 patients with interstitial pneumonia (IP), of which 21 were positive for p-ANCA and anti-MPO. p-ANCA+ patients were evenly distributed between idiopathic interstitial pneumonia (IIP) and IPAF. Compared to p-ANCA- patients, p-ANCA+ patients more often had non-specific interstitial pneumonia (NSIP) pattern, bronchiectasis, higher CRP, and arthralgias (Table 1A). Then we stratified our patient according to both ANCA positivity and pneumological diagnosis (Table 1B). IP pANCA+ group had a higher percentage of males (p=0.04) and NSIP HRCT pattern (p=0.02). At 6 and 12 months, IP pANCA+ patients showed higher frequency of bronchiectasis at 6 (p=0.02) and 12 months p=0.04).
None of the p-ANCA- patients developed vasculitis, but 29% and 38% of p- ANCA+ patients developed vasculitis at 6 and 12 months, respectively. No differences were observed in terms of HRTC progression, O2 therapy and death. Multiple regression models showed that disease duration was associated with HRCT progression (OR 1.28, p=0.03), smoke with death (OR 26.7, p=0.01), IPF with need of oxygen therapy (OR 6.33, p=0.04), ANCA positivity with the develop vasculitis (OR 1.22,p=0.04)
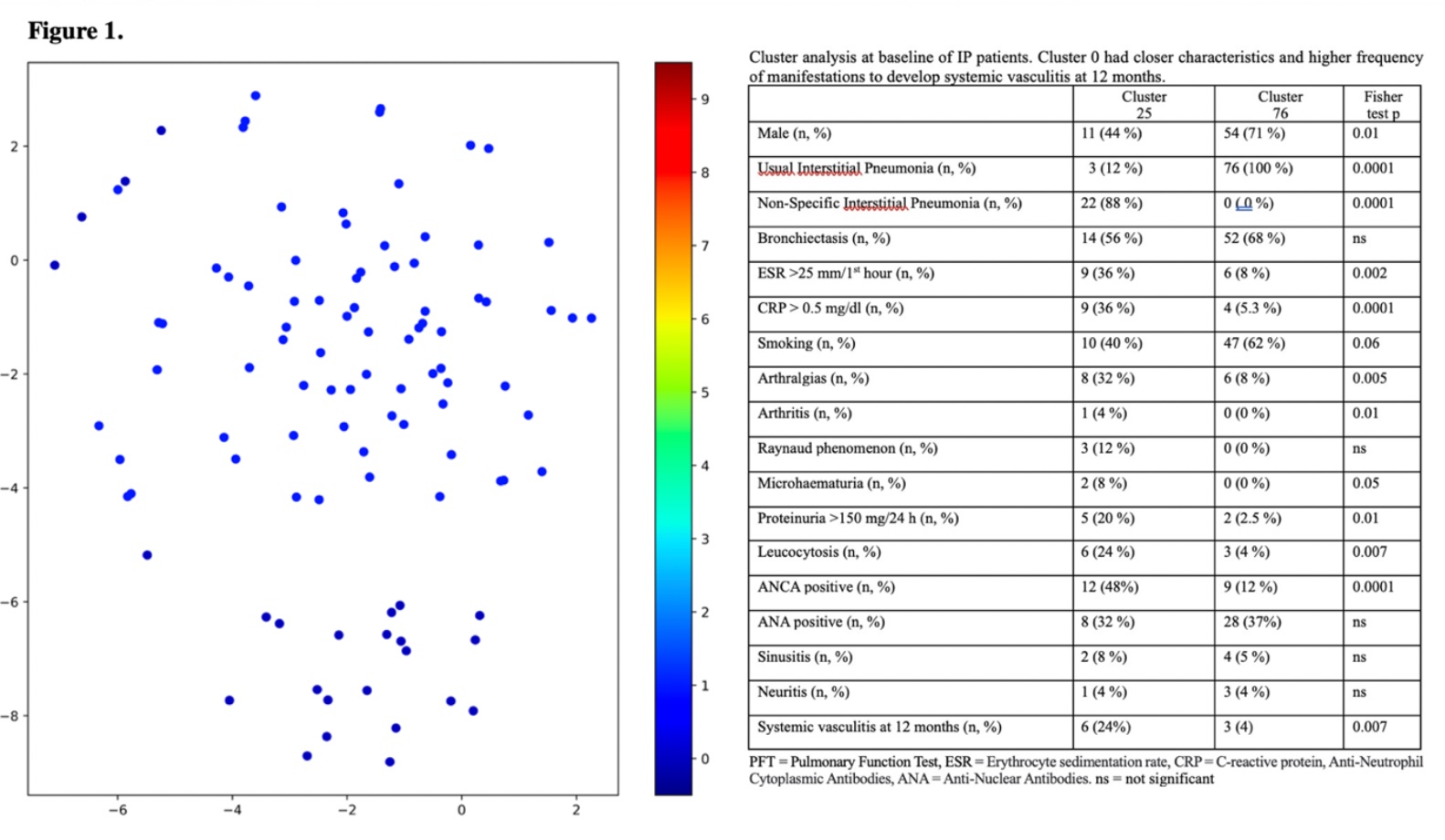
Unsupervised cluster analysis identified one group of 25 patients with significant higher NSIP (88%), ANCA+ (48%), arthralgias (32%) at baseline, and SV (24%) at 12 months (Figure 1).
Conclusion: These findings suggest that in patients presenting with IP, testing for ANCAs should be performed routinely, as positive anti-MPO along with some systemic manifestation may identify a cluster of patients at high risk of vasculitis. Whether IP-ANCA+ disease should be considered a new pathological entity needs further investigation on prospective cohorts.
To cite this abstract in AMA style:
Pellico M, Iannone C, Caminati A, Cassandro R, Colleoni M, Elia D, Luisi F, Mirenda M, Tescaro L, Zompatori M, Harari S, Caporali R. Anti-neutrophil Cytoplasmic Antibodies Associated Interstitial Pneumonia: A New Clinical Entity? [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/anti-neutrophil-cytoplasmic-antibodies-associated-interstitial-pneumonia-a-new-clinical-entity/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/anti-neutrophil-cytoplasmic-antibodies-associated-interstitial-pneumonia-a-new-clinical-entity/