Session Information
Session Type: ACR Concurrent Abstract Session
Session Time: 9:00AM-10:30AM
Background/Purpose: Data support that anti-CCP antibodies likely originate at a mucosal site prior to the onset of inflammatory arthritis (IA) in the development of RA. Our group identified anti-CCP in the lungs of subjects without IA who are At-Risk for future RA. However, a portion of serum CCP+ subjects did not exhibit anti-CCP in the lung, suggesting another mucosal site of generation. Based on a higher incidence of RA in women, the dynamic nature of immune responses in the cervicovaginal (CV) mucosa and our preliminary data that serum anti-CCP-IgG is associated with intrauterine device (IUD) use in first-degree relatives (FDR) of RA patients, we sought to evaluate anti-CCP antibodies in the CV mucosa of women with and without RA.
Methods: We studied premenopausal women: 11 serum CCP+ with classified RA, 18 At-Risk for RA (15 serum CCP- FDRs and 3 serum CCP+ from clinics) and 35 serum CCP- healthy Controls. A CV fluid (CVF) sample was collected between days 14-28 of the menstrual cycle. Paired serum and CVF was tested by ELISA for CCP3 (IgG, Inova). In 24 of the non-RA women, CVF was also tested for 11 inflammatory cytokines/chemokines (Meso Scale). In addition, 7 Controls collected serial CVF samples from 3 different menstrual cycle phases. No interference by hemolysis was found on CVF CCP results.
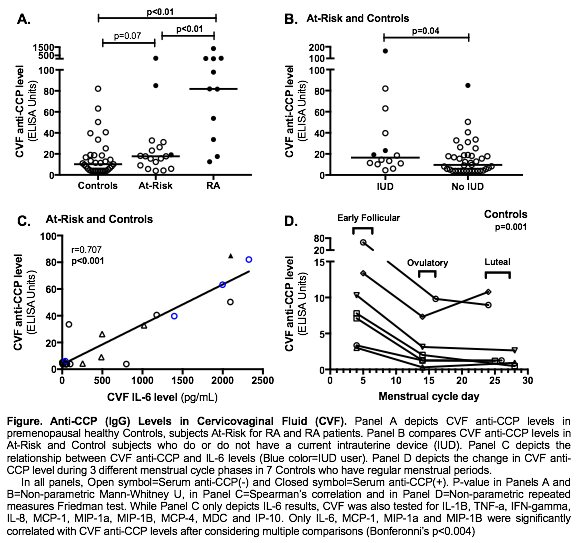
Results: CVF anti-CCP levels were higher in RA (Figure Panel A). In non-RA subjects, CVF anti-CCP levels were higher in current IUD users (p=0.04 in all non-RA; p=0.04 in Controls only; Panel B). There was no association between CVF anti-CCP levels and self-report of smoking, pregnancy, genital infection or other contraception type. In non-RA subjects, CVF anti-CCP significantly correlated with CVF markers of inflammation including IL-6, monocyte chemoattractant protein (MCP)-1, macrophage inflammatory protein (MIP)-1α and MIP-1β (p≤0.001 for all; Panel C shows IL-6). In addition, CVF anti-CCP was higher in the early follicular phase compared to ovulatory and luteal phases (p=0.001, Panel D), and in 4 Controls that were tested, CVF IL-6, MIP-1α and MIP-1β increased with anti-CCP levels in the early follicular phase.
Conclusion: We demonstrate for the first time that anti-CCP antibodies are elevated in CVF of women with and without RA. Importantly, these elevations were associated with markers of local CV inflammation. Furthermore, the 2 factors associated with higher CVF anti-CCP levels were IUDs and the early follicular phase, and both have previously been associated with local CV inflammation (Shanmugasundaram 2016; Macneill 2012). Of note, several serum CCP- women had elevated CVF anti-CCP levels suggesting that the CV mucosa may be a unique site of anti-CCP generation in some women, which could provide insight into the higher rates of RA in women. Additional studies are needed to identify specific mechanisms of CV anti-CCP generation and factors associated with transitions to systemic autoimmunity.
To cite this abstract in AMA style:
Khatter S, Berens-Norman H, Anderson C, August J, Feser ML, Fleischer C, Visser A, Norris JM, Holers VM, Deane KD, Demoruelle MK. Anti-CCP Antibody Levels Are Elevated in Cervicovaginal Fluid in Association with Local Inflammation in Premenopausal Women without RA [abstract]. Arthritis Rheumatol. 2017; 69 (suppl 10). https://acrabstracts.org/abstract/anti-ccp-antibody-levels-are-elevated-in-cervicovaginal-fluid-in-association-with-local-inflammation-in-premenopausal-women-without-ra/. Accessed .« Back to 2017 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/anti-ccp-antibody-levels-are-elevated-in-cervicovaginal-fluid-in-association-with-local-inflammation-in-premenopausal-women-without-ra/