Session Information
Date: Friday, November 6, 2020
Title: SLE – Diagnosis, Manifestations, & Outcomes Poster I: Clinical Manifestations
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: SLE is a systemic autoimmune disease notable for the ability to affect nearly every tissue, and is associated with a breadth of auto-antibodies. Anti-neutrophilic cytoplasmic antibodies (ANCA) are strongly associated with small-vessel vasculitis, specifically the ANCA-associated vasculitides, but their role in SLE is less clear. Purpose: To determine whether ANCA are associated with disease features including vasculitis in SLE.
Methods: Patients with 4 or more of the 1971 or 1982 ACR classification criteria, or 3 criteria and a typical biopsy of SLE are registered in the database and are followed longitudinally, with clinical and laboratory information collected at 2-6‐month intervals.
SLE patients with at least 2 ANCA tests, between Aug 1979 (when ANCA became locally available) and Nov 2019 were included. Patients with 2 consecutive ANCA (both C and P ANCA) were considered exposed in this study. Controls were patients who never had a positive ANCA. Index date was the time of the second ANCA. Vasculitis was defined by the SLEDAI-2K: ulceration, gangrene, tender finger nodules, periungual infarction, splinter hemorrhages, and biopsy/angiogram. Descriptive statistics were used to show patients’ characteristics at ANCA positive or negative in patient groups, Kaplan-Meier survival curves were plotted for outcomes of first vasculitis, Weibull parametric survival regression was applied to evaluate the effects of ANCA positivity on the outcome of vasculitis adjusting other confounding variables.
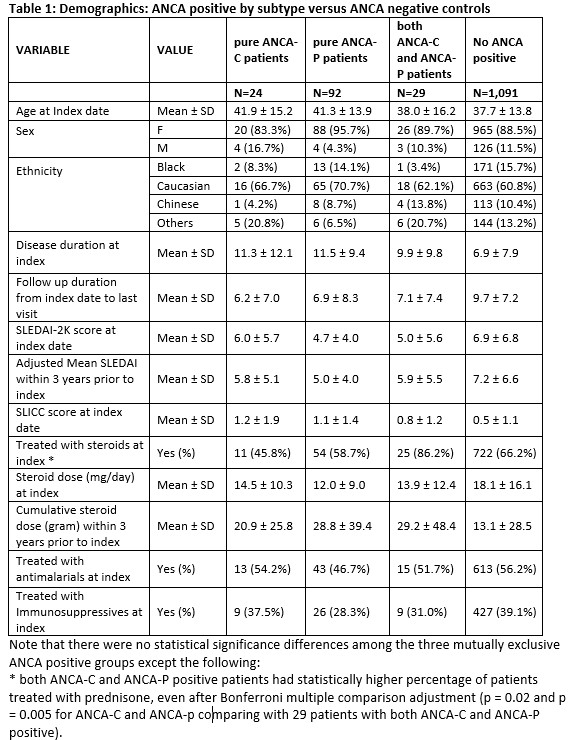
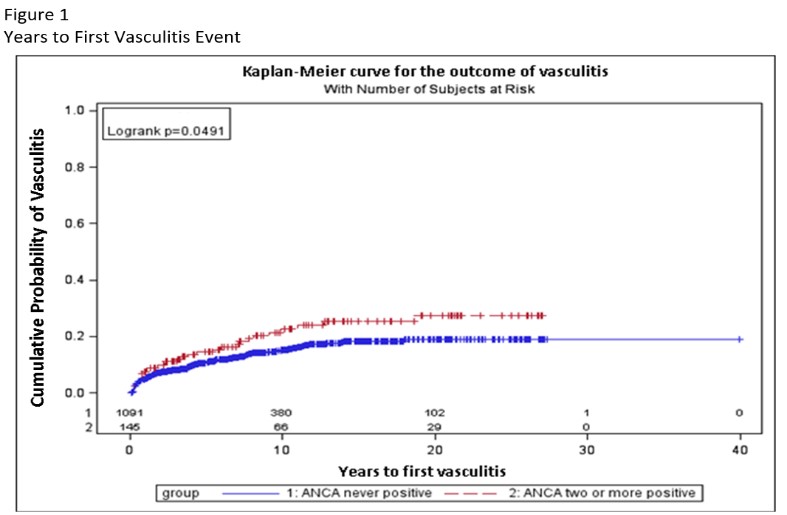
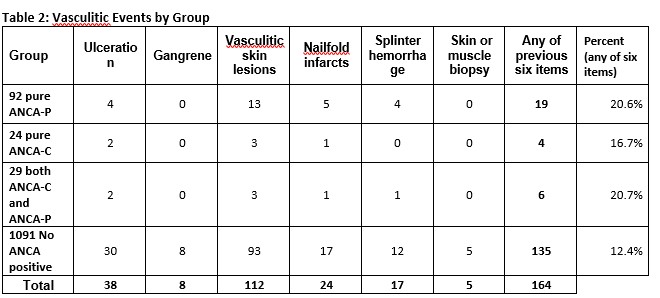
Results: Of the 1426 patients tested for ANCAs on two occasions, 1091 (77%) had never tested positive, 145 (10%) tested positive twice and 190 (13%) tested positive once. Those that tested positive twice or more included 92 with only p-ANCA, 24 with only c-ANCA, and 29 with both. Median time between first and second ANCA was 12 months. Patients’ demographics, clinical measurements, treatments are presented by ANCA subtype in table 1. Patients with either two positive ANCA-C or two positive ANCA-P had lower proportions of steroid treatment compared to 29 patients with both ANCA-C and ANCA-P positive, but were otherwise largely similar to those with both ANCA-C and ANCA-P positivity. Kaplan-Meier survival curves show significantly higher cumulative index of vasculitis in the 145 patients with any ANCA positive compared to none (p=0.0491, Figure 1). Survival regression models revealed that two or more ANCA-P positive (vs. normal ANCA patients) predicted the outcome of vasculitis after adjusting for SLEDAI-2K and prednisone treatment at index date (HR 1.78, 95% CI: 1.15-2.79) in the best fit multivariable model, while two or more ANCA-C positive did not reach significance in the other regression model. Looking into the nature of vasculitis, the proportion of patients with vasculitis within each of the ANCA subgroups were similar (p-ANCA 20.1%, c-ANCA 16.7%, mixed ANCA 20.7%), but only the p-ANCA group was significantly higher than those with no ANCA positivity (12.4%; Table 2) partially due to sample sizes.
Conclusion: In our cohort, approximately 10% of SLE patents have persistent ANCA positivity, predominantly p-ANCA. The presence of p-ANCA was associated with significantly more vasculitis predominantly skin vasculitis.
To cite this abstract in AMA style:
Mirza R, Urowitz M, Su J, Gladman D. ANCA in SLE: Prevalence and Predictor Factors [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/anca-in-sle-prevalence-and-predictor-factors/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/anca-in-sle-prevalence-and-predictor-factors/