Session Information
Date: Saturday, November 16, 2024
Title: Muscle Biology, Myositis & Myopathies – Basic & Clinical Science Poster I
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Dermatomyositis is an idiopathic inflammatory myopathy with proximal muscle weakness and skin manifestations. Myositis patients have poor overall health partially due to co-morbidities. Data on the co-occurrence of dermatomyositis and diabetes is limited, with most research focusing on the juvenile population. Moreover, long-term glucocorticoid (GC) use for dermatomyositis poses a risk of diabetes. Our study aimed to analyze the prevalence of diabetes in adult-onset dermatomyositis independent of GC use, determine associations with myositis-specific and myositis-associated antibodies, and identify the risk factors for diabetes in dermatomyositis. Additionally, we compared the dermatomyositis cohort to a matched control cohort to study the relationship between diabetes and dermatomyositis.
Methods: The Cleveland Clinic database was analyzed for a cohort of patients with dermatomyositis using ICD-10 code M33.1 from January 1, 2007, to December 31, 2021. A retrospective chart analysis identified patients with concurrent diabetes using the American Diabetes Association criteria. We analyzed the temporal association between dermatomyositis diagnosis, diabetes diagnosis, and GC initiation. The same database was used to find a control group of non-dermatomyositis patients seen during the same period. The chi-squared test compared diabetes prevalence in dermatomyositis to the control group. Logistic regression identified diabetes risk factors in dermatomyositis. We identified 434 dermatomyositis and 3,195,312 control patients. Out of these two groups, using propensity score matching in a 1:2 ratio based on age, body mass index (BMI), sex, race, smoking, hypertension, and dyslipidemia, 419 dermatomyositis patients were matched to 838 controls to study the impact of dermatomyositis on diabetes.
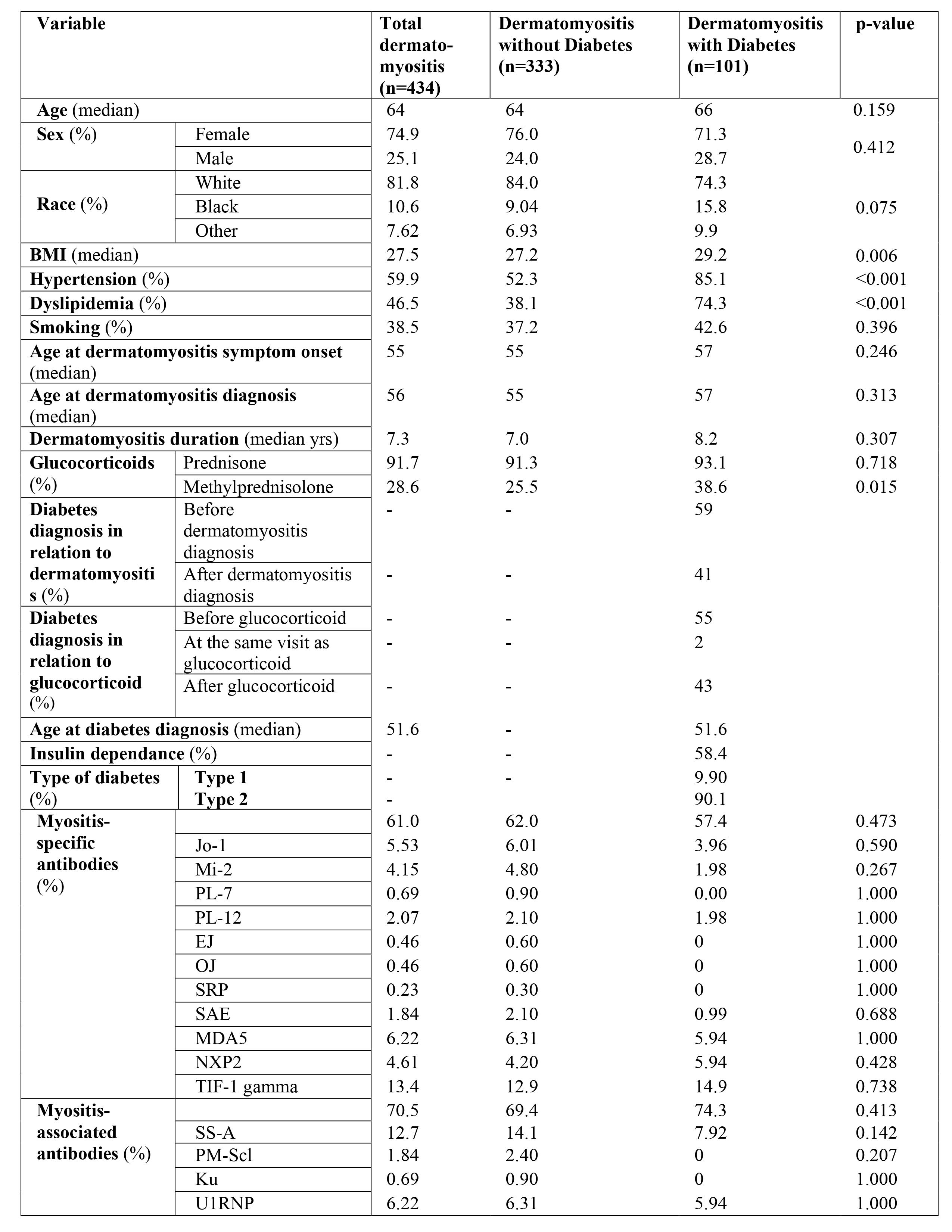
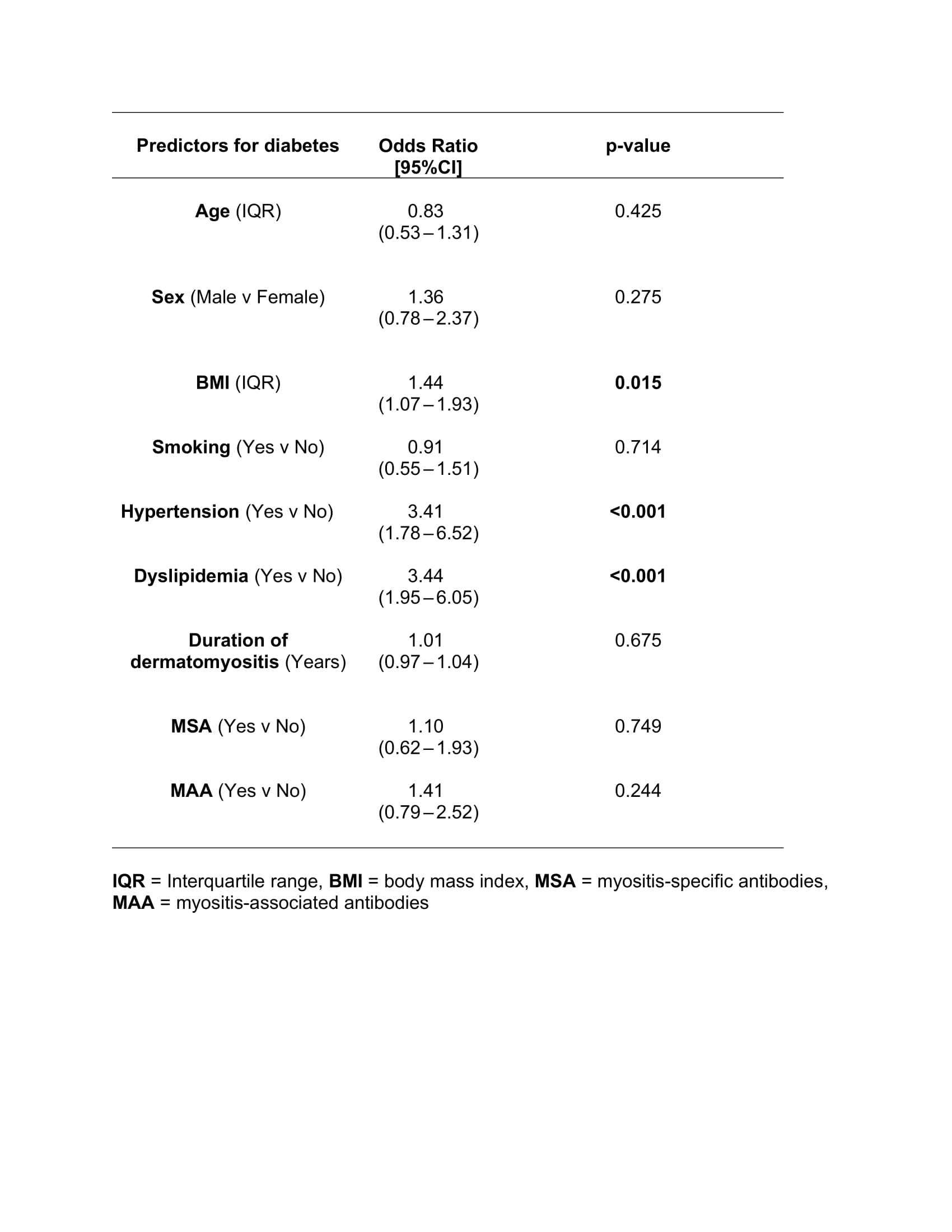
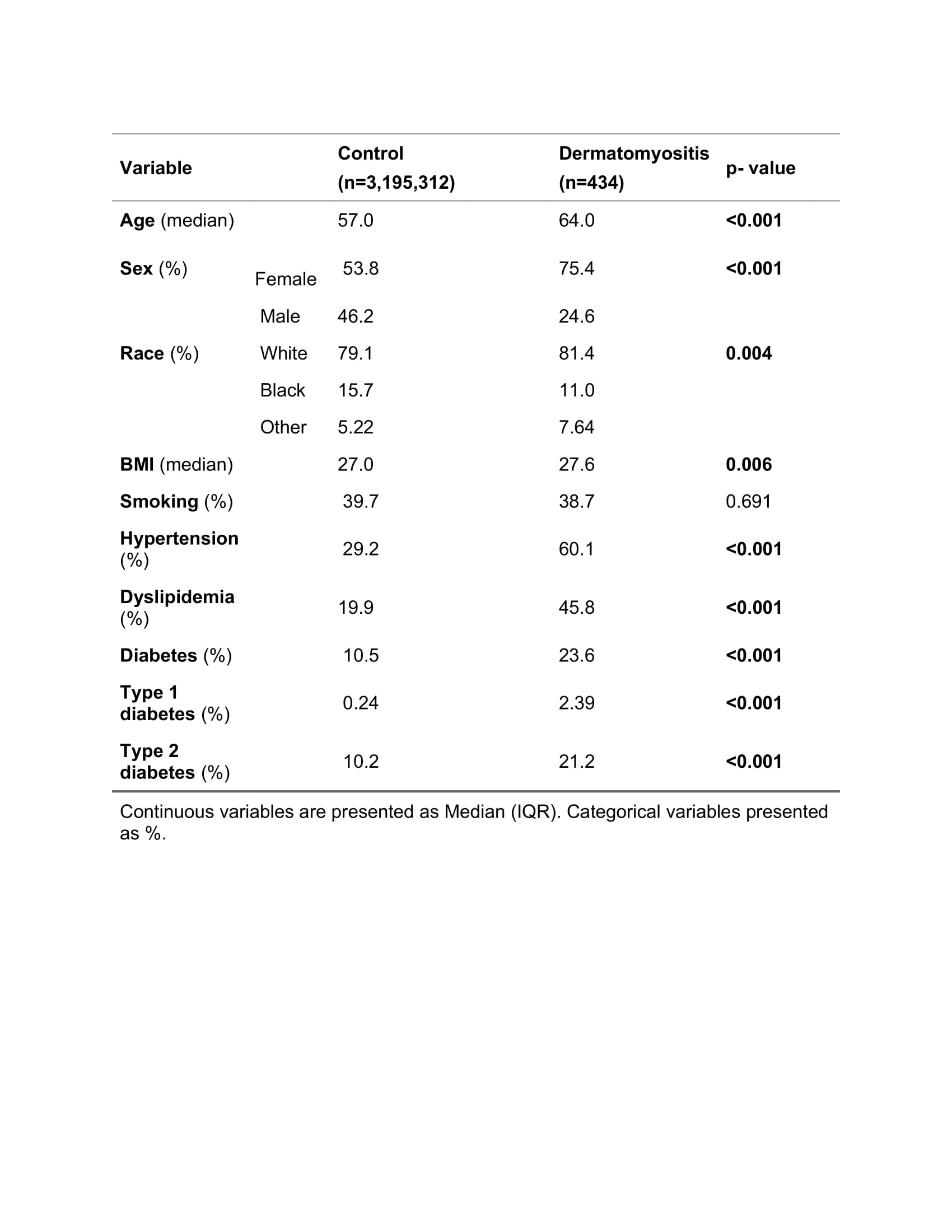
Results: The dermatomyositis cohort comprised 434 patients, predominantly female and Caucasian, with a median age of 64. The median ages at dermatomyositis symptom onset and diagnosis were 55 and 56, respectively. In this cohort, 59% were diagnosed with diabetes before dermatomyositis and 41% afterward. Of the cohort, 55% had diabetes before starting GC, 2% were diagnosed at the time of GC initiation, and 43% were diagnosed after GC use (Table 1). Among them, 90.1% had type 2 diabetes, and 58.4% were insulin dependent. Factors significantly associated with diabetes development included BMI, hypertension, and dyslipidemia, with no significant correlation with myositis-specific or associated antibodies (Table 2). The dermatomyositis cohort had a higher prevalence of not only diabetes (23.6% vs. 10.5%, p< 0.001) but also hypertension (60.1% vs. 29.2%, p< 0.001) and dyslipidemia (45.8% vs. 19.9%, p< 0.001) compared to unmatched control (Table 3). Dermatomyositis increased the odds of having diabetes by 7% compared to matched control (OR 1.07, p = 0.003).
Conclusion: This study highlights the higher prevalence of diabetes in adult-onset dermatomyositis, independent of GC use. Risk factors include hypertension, dyslipidemia, and high BMI. The findings underscore the need for early screening for diabetes, hypertension, and dyslipidemia to reduce cardiovascular risk in dermatomyositis patients.
To cite this abstract in AMA style:
Ejaz K, Zhang C, Chatterjee S. Analysis of the Prevalence of Diabetes Mellitus in Patients with Adult-onset Dermatomyositis [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/analysis-of-the-prevalence-of-diabetes-mellitus-in-patients-with-adult-onset-dermatomyositis/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/analysis-of-the-prevalence-of-diabetes-mellitus-in-patients-with-adult-onset-dermatomyositis/