Session Information
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Relapses are correlated with increased hospitalizations, poor renal outcomes, morbidity and mortality. We aim to investigate the incidence, predictive factors and outcomes related to renal relapse.
Methods: All patients with biopsy-proven LN (ISN/RPS 2003) with complete clinical data were included.
Demographic, clinical and laboratory data were obtained from the existing database and revised, especially for the renal parameters. The clinical status (complete response (CR), partial response (PR), and nonresponse (NR) ) was determined at the 6th and 12th months and at the last doses of induction, maintenance and re-induction therapies. CR was defined as UPCR < 0.5 g/g and PR was a reduction in the UPCR of ≥50% and < 3 g/g on early morning urine. Both CR and PR required improvement or stabilization of kidney function. NR was defined as failure to attain CR/PR at the given time. Renal relapse was defined as a UPCR >1 g/g in patients with baseline proteinuria < 0.5 g/g or an increase in UPCR by ≥1 g/g in patients with baseline proteinuria >0.5 g/ g and/or an increase serum creatinine. DORIS complete remission was described as a clinical SLEDAI=0, no serological activity, and no treatment with glucocorticoids or immunosuppressive (IS). LLDAS was defined as a SLEDAI ≤ 4 with no activity in major organ systems, a daily prednisolone≤ 7.5 mg/day, and allowing for maintenance IS. Flares, death, chronic renal failure, permanent dialysis and transplantation were also recorded.
The association of clinical characteristics of the cohort with renal flares and outcome was investigated.
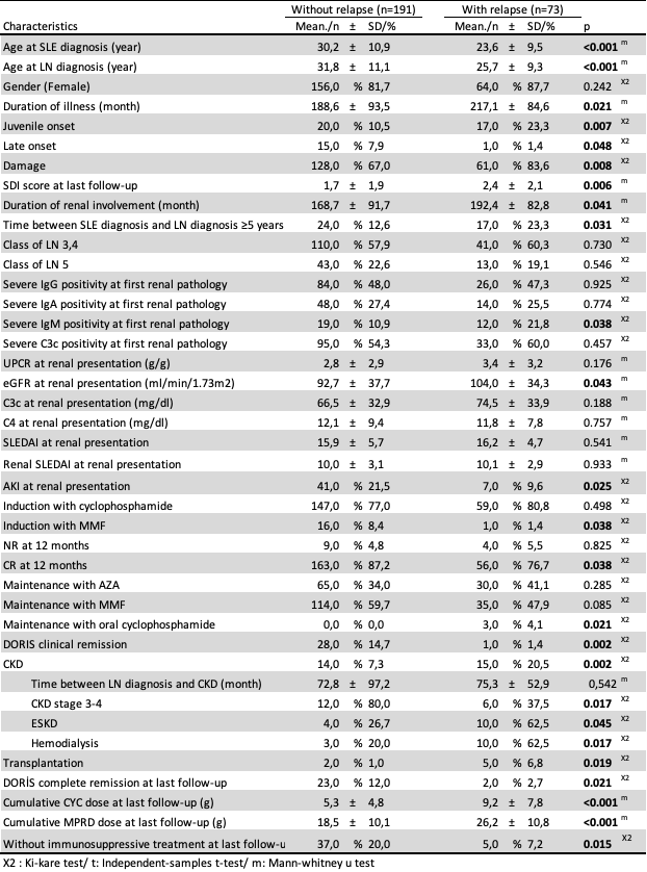
Results: Of 264 patients, 73 had relapsed. Mean glomerular filtration rate (GFR) was lower and the frequency of acute kidney injury (AKI) was higher in nonrelapsers at presentation. Comparison of groups showed no difference for the use of CYC, AZA, and RTX whilst frequency of MMF use at induction was less in relapsers. Compared with nonrelapsers, a lower proportion of relapsers achieved CR at 12 months. There was no difference between AZA and MMF as maintenance treatment. Relapsers showed a higher rate of chronic renal disease (CKD) and transplantation and had a lower DORIS complete remission rate.
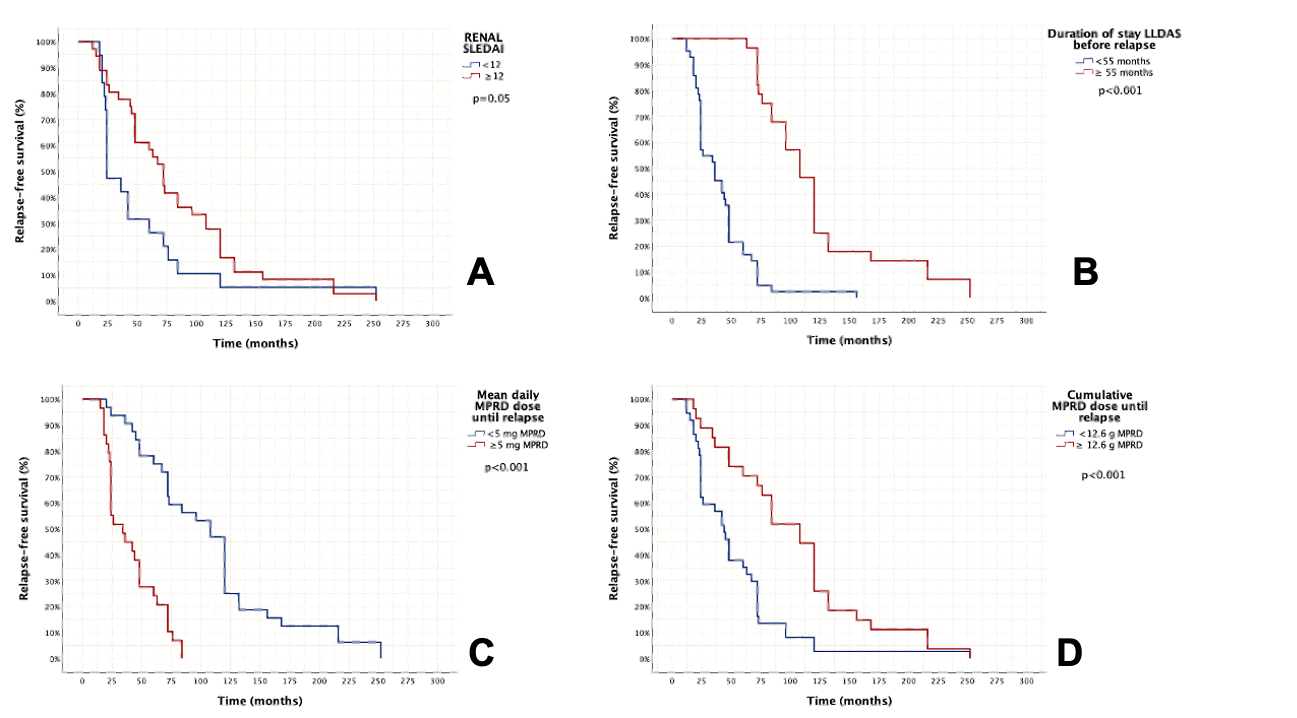
Multivariate analysis demonstrated that younger age at SLE diagnosis (p< 0.001), and severe IgM positivity in renal pathology (p=0.042) were significant risk factors for developing renal relapse. Renal SLEDAI at first presentation (p=0.021), duration stay in LLDAS ( p< 0.001), mean daily methylprednisolone (MPRD) (p< 0.001) and cumulative MPRD dose until first relapse (p=0.008) were significant risk factors for time to renal relapse. Relapsers had a higher damage score compared to nonrelapsers.
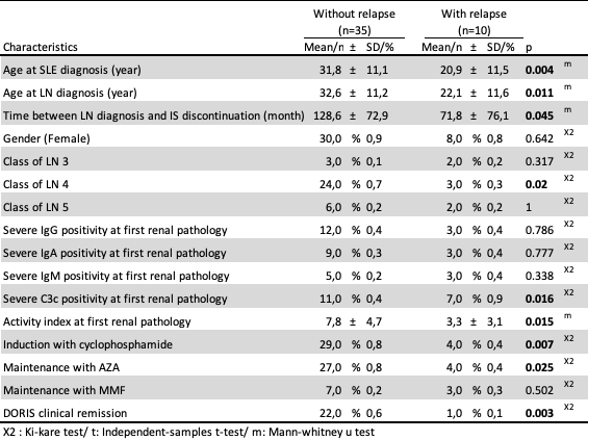
Upon discontinuation of IS treatment, the risk of relapse was higher at younger age of diagnosis ( p=0.042), and severe C3c positivity at renal pathology (p=0.033).
Conclusion: Preventing relapse is essential for preventing the development of CKD and damage. Patients with younger age at SLE and LN diagnosis, and severe IgM positivity at renal pathology are more prone to relapse. AKI in the renal presentation was associated with less relapse. It is important to not to discontinue IS treatment early especially in these high-risk patients.
To cite this abstract in AMA style:
Kemec G, Varelci S, Gurel E, Kılıcaslan I, özlük Y, Yalcınkaya Y, Gul A, Inanc M, Artım Esen b. Analysis of Relapses in a Single Center Cohort of Patients with Lupus Nephritis [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/analysis-of-relapses-in-a-single-center-cohort-of-patients-with-lupus-nephritis/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/analysis-of-relapses-in-a-single-center-cohort-of-patients-with-lupus-nephritis/