Session Information
Session Type: Poster Session (Sunday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Cardiac involvement in Spondyloarthritis (SpA) has been recognised as an important determinant of increased comorbidity and mortality due to atherosclerosis, aortitis, aortic regurgitation and ventricular dysfunction. Cardiac conduction abnormalities are commonly noted and may occur prior to symptom onset.
One potential relationship that warrants further study is with Brugada Syndrome (BrS). This is a rare inherited cardiac disorder characterised by disturbances of the conduction system of the heart. The clinical presentation varies from being asymptomatic to syncope and sudden cardiac death (SCD) due to ventricular arrhythmias. BrS can be associated with mutations in the SCN5A gene in a fifth of cases, encoding the cardiac sodium channel alpha subunit leading to cardiac conduction defects.
Methods: A database search of patients diagnosed with BrS at one centre was performed. The diagnosis was made in line with international guidelines (1): the presence of a spontaneous or intravenous Ajmaline (class Ia antiarrhythmic) provoked type 1 or ‘coved’ electrographic (ECG) pattern with J point and ≥2mm concave ST elevation in at least one ECG lead V1/2 recorded from the 4th,3rd and/or 2ndintercostal spaces; J point and ‘saddleback’ ST elevation with a positive T wave in at least one ECG lead V1/2 recorded from the 4th, 3rd and/or 2nd intercostal spaces (type 2/3: depending on degree of J point and ST elevation) if converted to a type 1 through Ajmaline induction. Documented ventricular fibrillation (VF) or polymorphic ventricular tachycardia (VT), syncope, family history of premature SCD and/or type 1 Brugada pattern was supportive. A validated genetic screen was done. All patients who were also under Rheumatology were identified. An interrogation of their medical records was conducted to extract: demographics, diagnosis of SpA, as defined by the Assessment of SpondyloArthritis International Society (ASAS) criteria, other rheumatology diagnoses, and other co-variates.
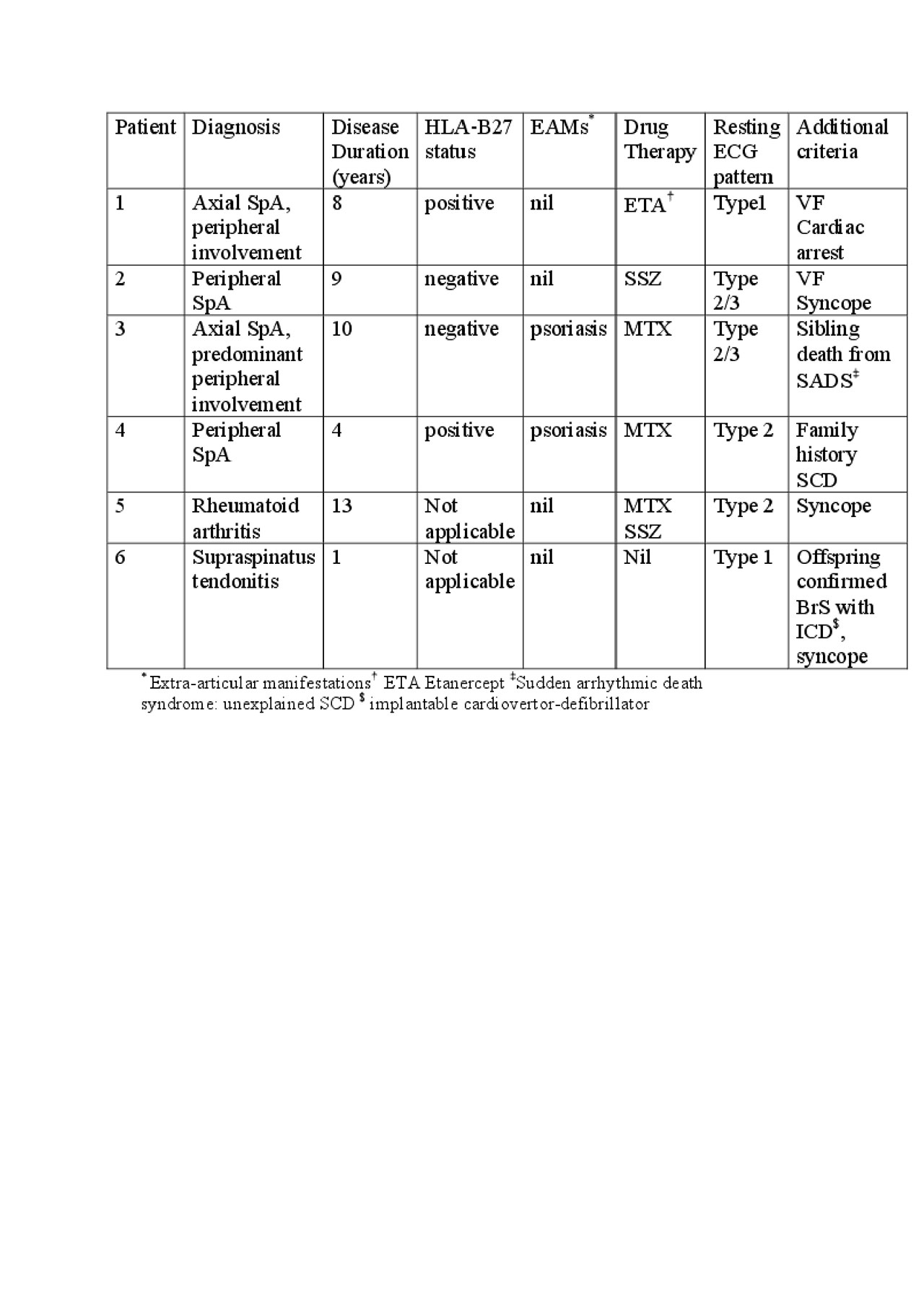
Results: Of the 600 patients diagnosed with BrS, n=6, were found to have attended Rheumatology. There were 4 females and 2 males with a mean age= 52.1 years (30-71).
The Table shows the main findings.
All patients demonstrated a Type 1 Brugada pattern during the provocation test or spontaneously. All had structurally normal hearts on echocardiography and cardiac MRI at diagnosis. None of the patients had the SCN5A mutation. Patients 1 and 2 had an ICD device fitted as a consequence. All were given preventative lifestyle advice in the form of avoidance of excess alcohol, illicit substances, arrhythmogenic drugs, treating fever promptly with anti-pyretics and keeping hydrated.
Conclusion: There appears to be a preponderance of patients with peripheral SpA who have BrS (0.67%) compared to expected Caucasian and SE Asian population frequencies of 0.05% and 0.2% respectively. Half of the cases were HLA-B27 positive. Aside from psoriasis, there were no other EAMs noted. Whether this reflects inflammatory activity or a genetic link is unclear. This analysis highlights a potential important relationship, which requires further study.
References: Priori, S.G., et al., Heart Rhythm, 2013. 10(12): p.1932-63
To cite this abstract in AMA style:
Lall K, Ramsden R, Behr E, Sandhu V. An Observational Analysis of the Co-existence of Brugada Syndrome in Patients with Spondyloarthritis; A Potentially Important Link [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/an-observational-analysis-of-the-co-existence-of-brugada-syndrome-in-patients-with-spondyloarthritis-a-potentially-important-link/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/an-observational-analysis-of-the-co-existence-of-brugada-syndrome-in-patients-with-spondyloarthritis-a-potentially-important-link/