Session Information
Session Type: Poster Session (Monday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Systemic Lupus Erythematosus (SLE) is a chronic multisystem autoimmune disorder with variable presentation. While several studies have outlined the risk factors for hospitalization and mortality in SLE, the frequency of these causes have varied among studies and over the years. We aimed to assess leading nationwide causes of SLE hospitalizations and mortality in the US in a recent year, 2016 using a large inpatient database.
Methods: We used the National Inpatient Sample (NIS) database from the year 2016 to identify hospitalizations with SLE using the previously validated International Classification of Disease (ICD-10) code M32. NIS is a part of the Healthcare Cost and Utilization Project (HCUP). It contains 20 % stratified sample of US hospital discharges (~ 7 million/year), the weighted estimate of which corresponds to about ~ 35 million/year. Hospitalizations with SLE in primary and secondary positions were identified. Among SLE as the secondary diagnosis, ICD-10 codes used to look for primary diagnoses associated with hospitalizations and mortality.
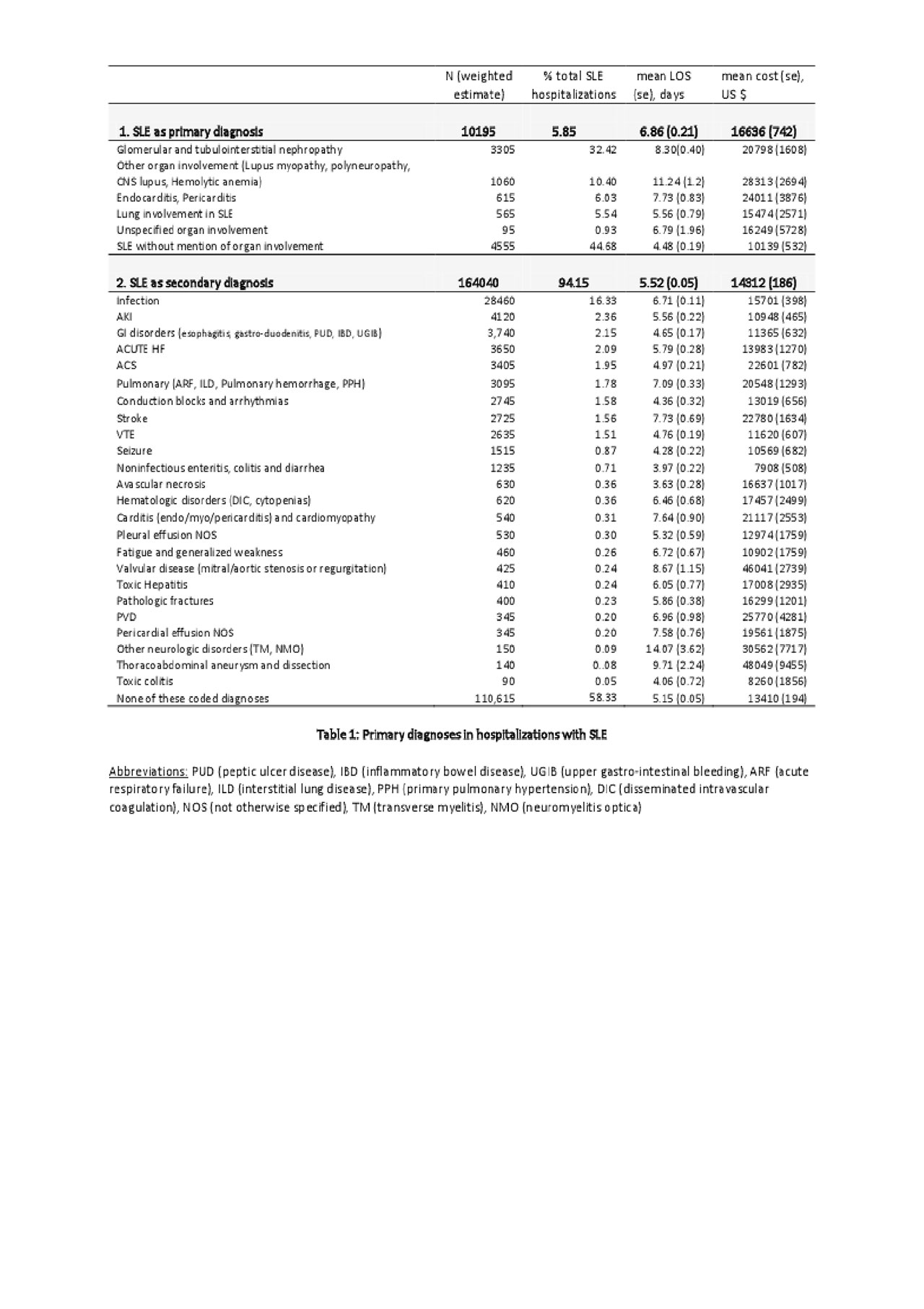
Results: We identified 174,235 SLE hospitalizations in 2016 among which 89% were females. The mean age of hospitalization for SLE was 52 years and mean length of stay was 5.6 days. SLE was the primary diagnosis in 10,195 (5.85%) patients, among which lupus nephropathy was the most common (32.42%). Among SLE as the secondary diagnosis, infection was the commonest primary diagnosis (16.33 %) followed by acute kidney injury (2.36%) and gastrointestinal manifestations (2.15%). Cardiac manifestations including acute heart failure (2.09%), acute coronary syndrome (1.96%) and conduction disturbances (1.58%) were other important causes of hospitalization (Table 1). In-hospital mortality of SLE was 1.95% and infection was the leading cause of in-hospital mortality (38%) (Table 2).
Conclusion: In our study using a large national database, we noted that SLE was the primary cause for hospitalization in 5.85 %, which is fewer than previously reported. Infection was the leading primary diagnosis associated with SLE hospitalization, which is in accordance with other recent studies globally. On 2016, the inpatient mortality for SLE was 1.95 %, which was fewer than the 3.15% reported by Krishnan et al. using the same NIS database (1998 – 2002), which suggests possible improvement in mortality in SLE hospitalizations in the recent years. In conclusion, infection was the leading reason for hospitalization and in-hospital mortality in SLE. Renal and cardiac involvements were other important causes of hospitalization.
To cite this abstract in AMA style:
Dhital R, Poudel D, Pandey R, Karmacharya P. All-cause Hospitalizations and Mortality in Systemic Lupus Erythematosus in the US- results from a National Inpatient Database [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/all-cause-hospitalizations-and-mortality-in-systemic-lupus-erythematosus-in-the-us-results-from-a-national-inpatient-database/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/all-cause-hospitalizations-and-mortality-in-systemic-lupus-erythematosus-in-the-us-results-from-a-national-inpatient-database/