Session Information
Session Type: Poster Session D
Session Time: 1:00PM-3:00PM
Background/Purpose: Ultrasound is a promising non-invasive tool in the evaluation of the salivary glands for parenchymal changes related to Sjögrens Syndrome (SS). The OMERACT Ultrasound Grey-scale (GS) Scoring System for SS has been shown to have good sensitivity and excellent specificity for fulfilling the SS classification criteria, when a GS ≥2 in at least 1 gland was considered indicative of SS (1), however others have suggested pathology in at least 2 glands is required (2). Systematic use of ultrasound might reduce the need for labial biopsies if US findings are in agreement with biopsies.
The aim was to assess the agreement between labial biopsy results and salivary gland ultrasound findings in patients suspected of SS.
Methods: Patients referred to our department with a suspicion of SS from 2017-2021, scheduled for a diagnostic labial biopsy were recruited. All underwent GS ultrasound of the parotid and submandibular glands bilaterally prior to clinical exam, Schirmer’s test, unstimulated salivary flow, blood samples including autoantibody analysis. Still images of the four glands were scored 0-3 using a previously developed ultrasound atlas (1) of the OMERACT ultrasound scoring system for SS (2,3). All biopsies were evaluated by a pathologist and focus score ≥1 was considered indicative of SS. Two different ultrasound scores for SS were tested: US-score ≥2 in at least 1 gland and US-score ≥2 in at least 2 glands. Descriptive statistics were used. In these analyses, we used labial biopsy as reference standard.
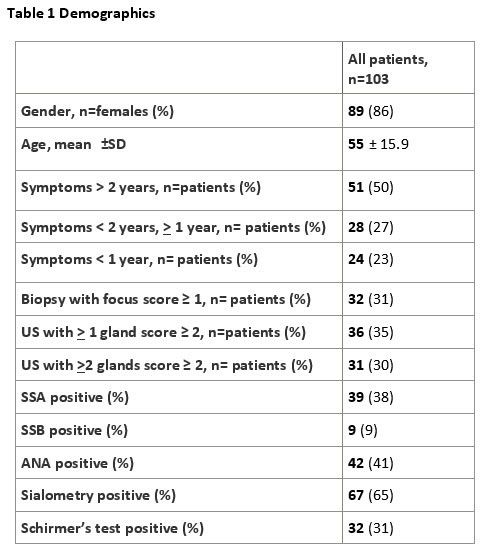
Results: 103 patients were included and 44 were clinically diagnosed with SS of which 42 (95%) fulfilled the 2016 ACR/EULAR classification criteria and 33 (75%) had positive labial biopsy. Demographics are shown in table 1.
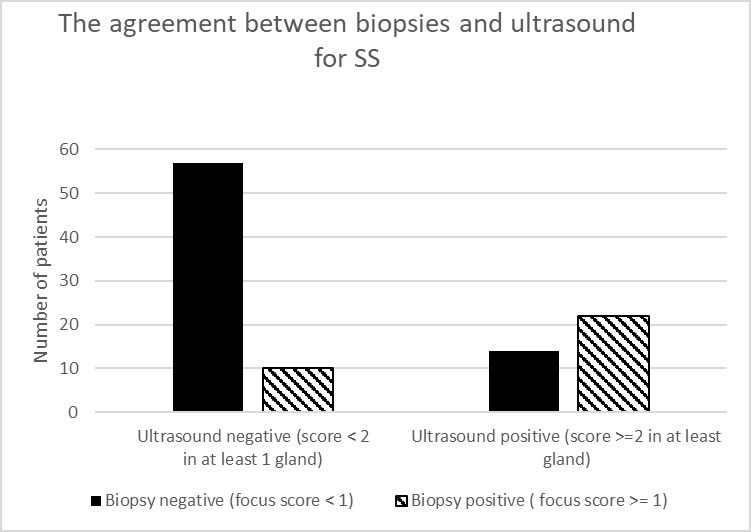
The sensitivity of ultrasound score ≥2 in at least 1 gland was 0.69 and the specificity 0.80. The positive predictive (PPV) and negative predictive values (NPV) were 0.61 and 0.85, respectively. Applying ultrasound score ≥2 in at least 2 glands did not improve specificity (0.83), PPV (0.61) or NPV (0.82) whereas sensitivity dropped to 0.59. The agreement between biopsies and ultrasound for SS is shown figure 1.
Conclusion: In patients with suspected SS, we found good agreement between US of salivary glands and subsequent labial biopsy. US of salivary glands seems useful in the diagnosis and classification of SS, but labial biopsies may still be needed in select cases.
To cite this abstract in AMA style:
Fana V, Schmidt N, Døhn U, Krabbe S, Terslev L. Agreement Between Labial Biopsy and the OMERACT Grey-scale Ultrasound Scoring System for Salivary Glands in a Single-center Cohort of Patients with Suspected Sjögren’s Syndrome [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/agreement-between-labial-biopsy-and-the-omeract-grey-scale-ultrasound-scoring-system-for-salivary-glands-in-a-single-center-cohort-of-patients-with-suspected-sjogrens-syndrome/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/agreement-between-labial-biopsy-and-the-omeract-grey-scale-ultrasound-scoring-system-for-salivary-glands-in-a-single-center-cohort-of-patients-with-suspected-sjogrens-syndrome/