Session Information
Session Type: Abstract Session
Session Time: 2:00PM-3:30PM
Background/Purpose: Ageism (stereotypes, prejudice or discrimination based on age) is highly prevalent and has been linked to reduced lifespan, prolonged disability, and accelerated cognitive decline in older adults. Very little is known about ageism within the field of rheumatology. The aim of this study is to understand ageism among rheumatology health care professionals and to assess how ageism affects rheumatologic care.
Methods: An English language REDcap survey, distributed over social media and email, included Likert scaled, multiple-response and free response questions related to the clinical care of older adults and the validated Expectations Regarding Aging (ERA-12) scale where higher scores indicate reduced stereotypical beliefs regarding aging. Spearman’s rank correlation coefficients were calculated for the ERA-12 scores and the responses to the other Likert questions to assess the effects of ageism on self-reported rheumatologic care decisions.
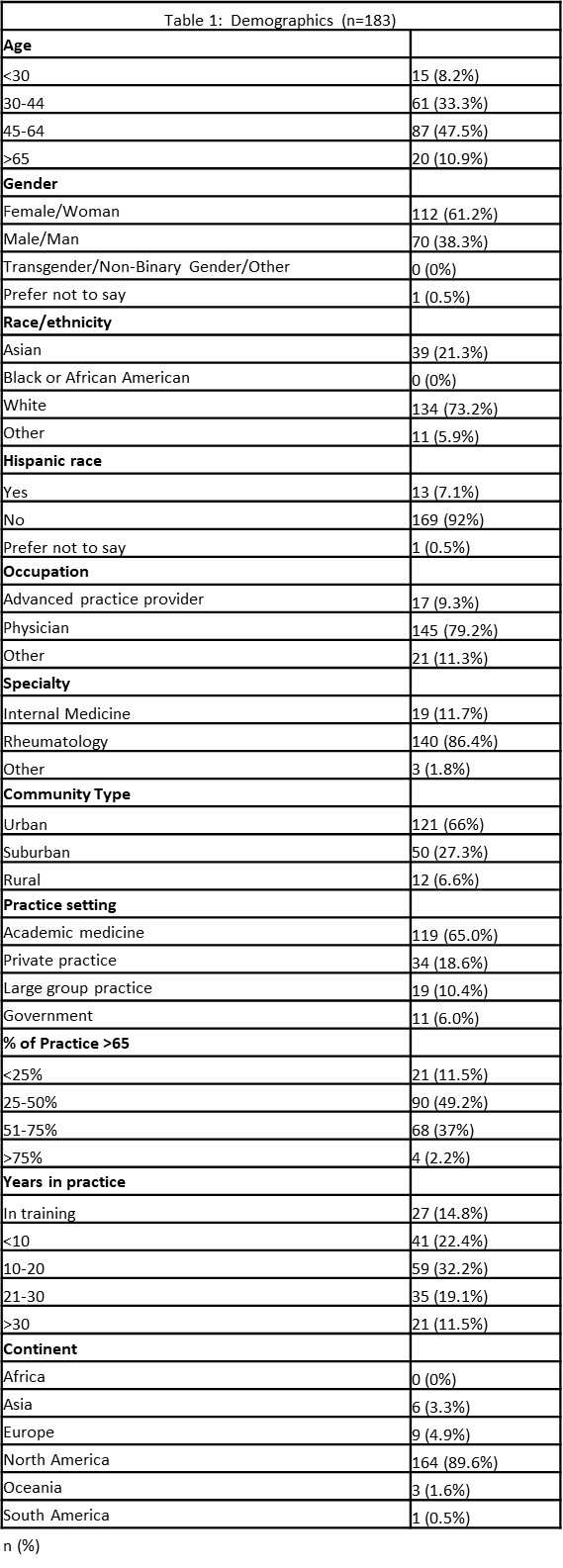
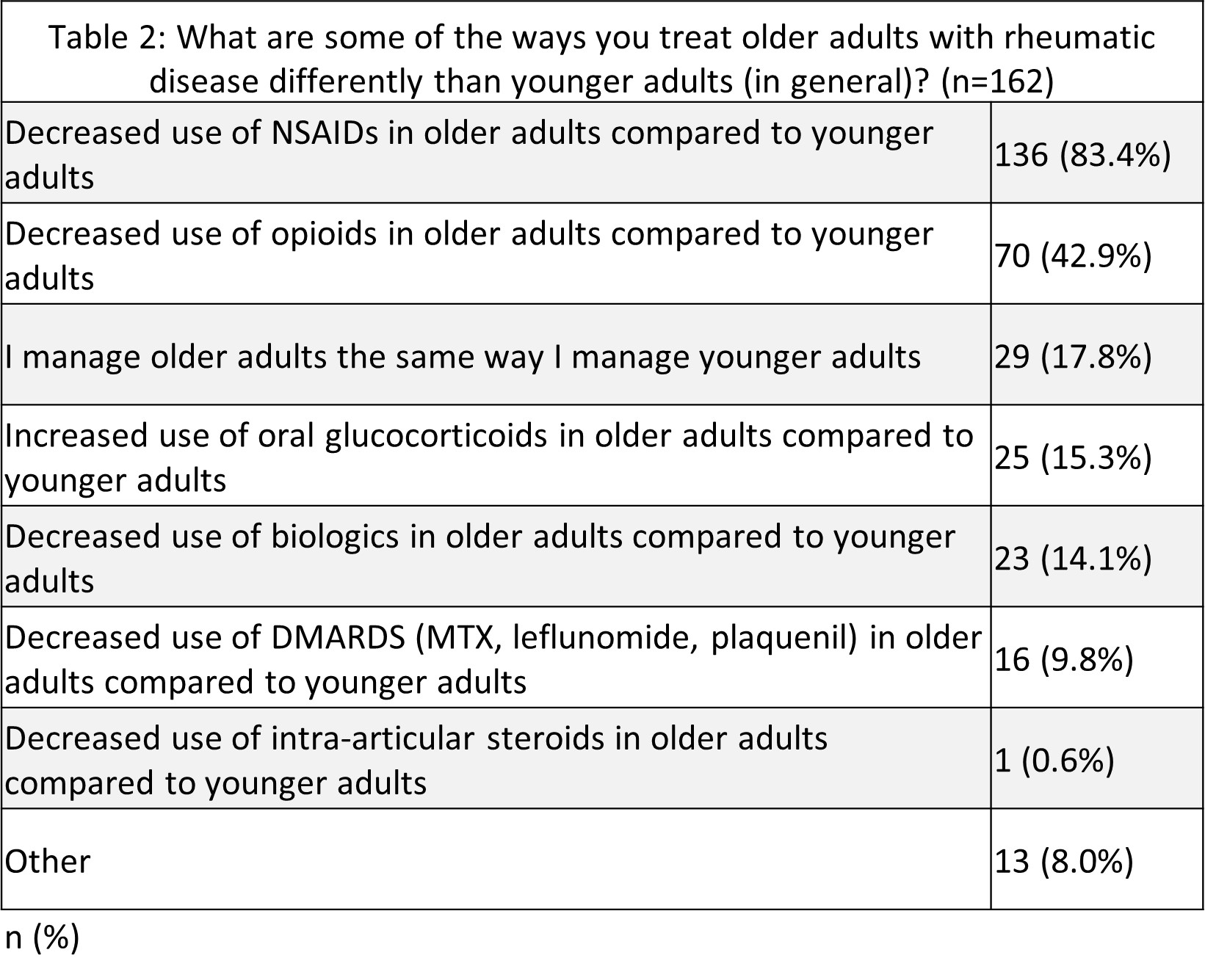
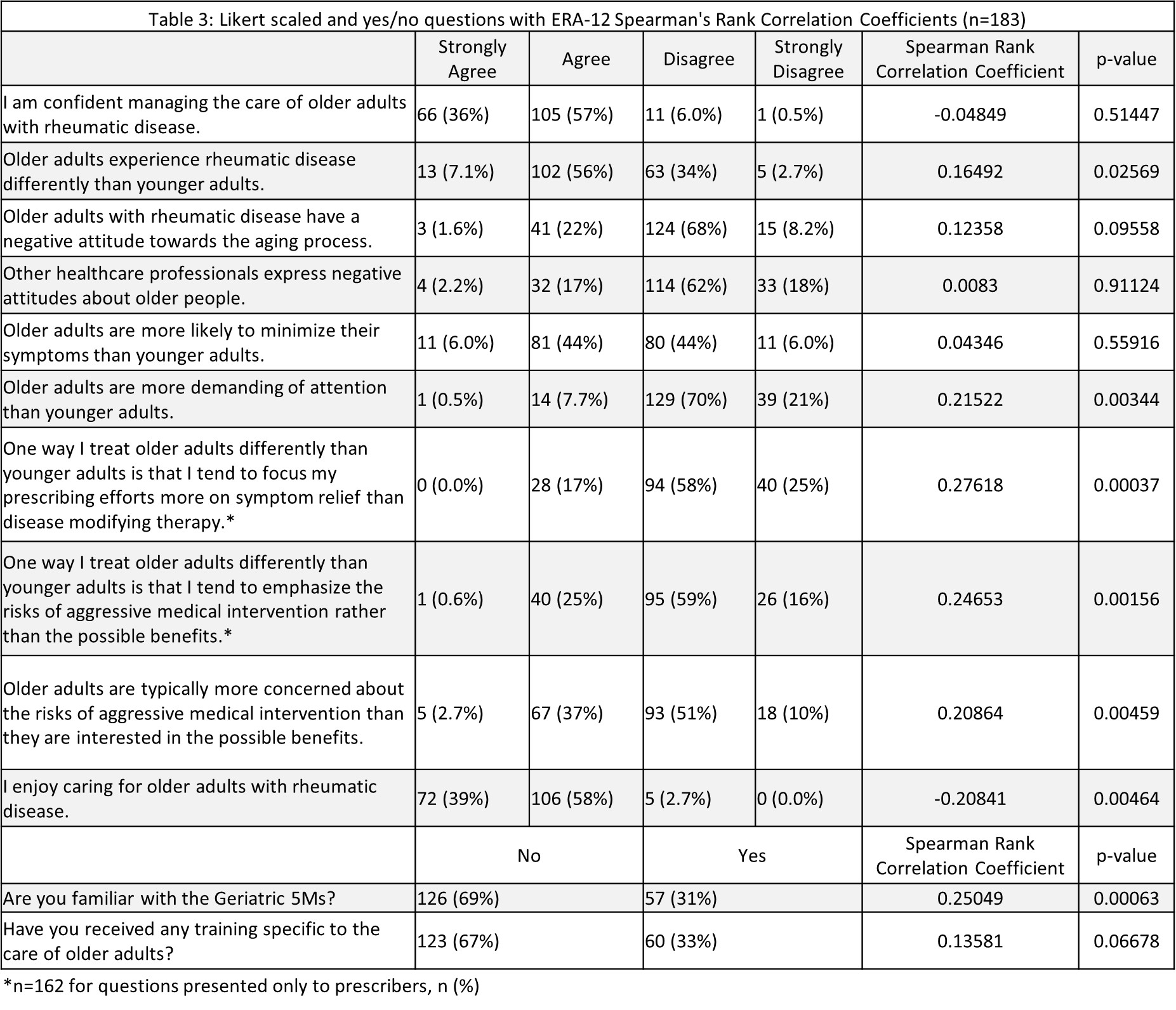
Results: Over 3 months, 183 surveys were completed by respondents around the world but predominantly in the US. The survey respondent median age was between 45-64, 61% were women, 73% were white and 51% had been in practice for >11 years (Table 1). Most respondents were physicians (79%), specializing in rheumatology (86%), and practicing in academic medicine (65%). The most challenging aspects of caring for older adults were reported to be multi-complexity (90%), polypharmacy (79%), insufficient visit time (53%) and patient financial limitations (45%). The most frequently reported differences in the care of older adults included reduced use of NSAIDs (83%) and decreased use of opioids (42%), with a minority of providers reporting that they manage older and younger adults the same (18%) (Table 2). The median ERA-12 score was 36 out of 48 indicating that respondents on average disagreed with the stereotypes regarding aging but did not strongly disagree. Table 3 shows higher ERA-12 scores (less ageist beliefs) were associated with greater enjoyment of the care of older adults (p=0.0046) and awareness of the Geriatrics 5Ms (p=0.00063). Lower ERA-12 scores were associated with believing that older adults are more demanding of attention (p=0.0034) and more concerned about the risks of medical therapy (p=0.0046) than younger adults. Lower ERA-12 scores were also associated with a shift from disease modifying therapy to symptom relief in older adults (p=0.00037).
Conclusion: Increased stereotypical thinking regarding aging is associated with self-reported changes to patient counseling, medical decision making, and perception of patient goals. This suggests that our biases regarding aging may affect how we care for older patients. Knowledge of the Geriatrics 5Ms was correlated with increased ERA-12 scores suggesting that increased awareness of aging principles may reduce these stereotypes and ultimately improve care for older adults. Further studies to quantify the effects of ageism on patient care and to assess the patient perspective on ageism in rheumatology are needed to identify interventions that can improve outcomes for this patient population.
To cite this abstract in AMA style:
Smith A, Achanta P, Makris U. Ageism in Rheumatology: The Health Care Professional’s Perspective [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/ageism-in-rheumatology-the-health-care-professionals-perspective/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/ageism-in-rheumatology-the-health-care-professionals-perspective/