Session Information
Date: Sunday, October 26, 2025
Title: (0593–0640) Systemic Lupus Erythematosus – Diagnosis, Manifestations, & Outcomes Poster I
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: The demographics of our lupus cohort have shifted over the decades towards an older population. While much of the shift can be attributed to advances in patient care leading to longer survival, we have also observed an increase in the age at which patients are being diagnosed with lupus. We examined this increase in the age of diagnosis and the impact on the disease manifestation profile.
Methods: The study was based on 3060 patients from a longitudinal SLE cohort in whom the date of SLE diagnosis was known (extracted from review of medical records), and who had at least 1 cohort visit. Patients were divided into 7 cohorts based on the decade of SLE diagnosis (1960-1969, 1970-79, 1980-89, 1990-99, 2000-09, 2010-2019, >2020). The catchment area of the cohort has remained Baltimore city and surrounding counties. The study incorporated all components of the 1997 ACR classification criteria for SLE (malar rash, discoid rash, photosensitivity, oral ulcers, arthritis, pleuritis or pericarditis, proteinuria, neurologic manifestations, hematologic manifestations, immunologic manifestations) to determine if there were differences in the percent of patients presenting with a given manifestation at the time of SLE diagnosis (and up to 1 year after diagnosis). For analysis of lupus manifestations we used Chi-squared tests (Pearson) and exact Cochran Armitage for trend.
Results: The average age of diagnosis steadily increased over time, from 21.0 years in the 1960’s to 40.2 years after 2020 (Figure 1). Similar increases were seen for Blacks, Whites and East Asians as well as females and males (Figure 1). For those diagnosed between 1990 to 2019, men were significantly older than women at diagnosis and Whites were significantly older than Blacks and East Asians at diagnosis (Table 1). Those diagnosed after 30 years of age were more likely to have oral ulcers, hematologic manifestations, immunologic manifestations and positive ANA, and less likely to have malar rash and proteinuria compared to those diagnosed before 30 years of age (Table 2). The same patterns for the ACR classification criteria were also observed at 5 years after diagnosis.
Conclusion: SLE has long been characterized as a disease with onset under 30. While diagnosis before the age of 30 years still predominates, diagnosis after the age of 30 has become more and more evident. SLE diagnosed in older adults exhibits a different profile of manifestations with less malar rash and proteinuria, but more hematologic and immunologic manifestations.
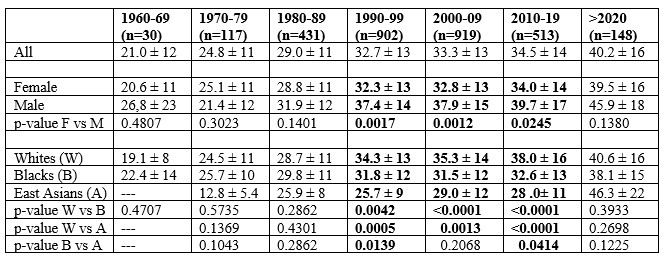 Figure 1 – Average Age of Diagnosis by Decade
Figure 1 – Average Age of Diagnosis by Decade
.jpg) Table 1. Age of Diagnosis by decade of diagnosis for demographic subgroups – mean ± SD (t-test).
Table 1. Age of Diagnosis by decade of diagnosis for demographic subgroups – mean ± SD (t-test).
.jpg) Table 2. Manifestations of SLE at Diagnosis, by Age at Diagnosis – Percent of total
Table 2. Manifestations of SLE at Diagnosis, by Age at Diagnosis – Percent of total
To cite this abstract in AMA style:
Goldman D, Fava A, Magder L, Petri M. Age at Diagnosis of SLE has Increased in a United States Longitudinal Cohort [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/age-at-diagnosis-of-sle-has-increased-in-a-united-states-longitudinal-cohort/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/age-at-diagnosis-of-sle-has-increased-in-a-united-states-longitudinal-cohort/
