Session Information
Date: Sunday, November 12, 2023
Title: (0460–0479) Reproductive Issues in Rheumatic Disorders Poster I
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Outside of the known association of Ro antibody with congenital heart block (CHB), little is known about adverse maternal outcomes, and even less about neonatal outcomes, in patients with Sjogren’s Disease (SjD).Few studies of pregnancy in SjD have been conducted in collaboration with Maternal Fetal Medicine (MFM). With an interdisciplinary approach, we aim to describe maternal and neonatal outcomes of pregnancies in SjD compared to a 1:3 matched control population.
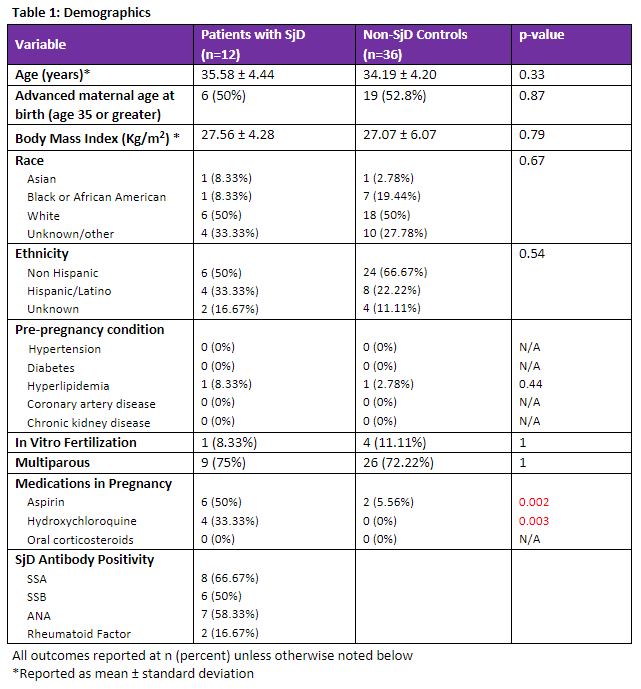
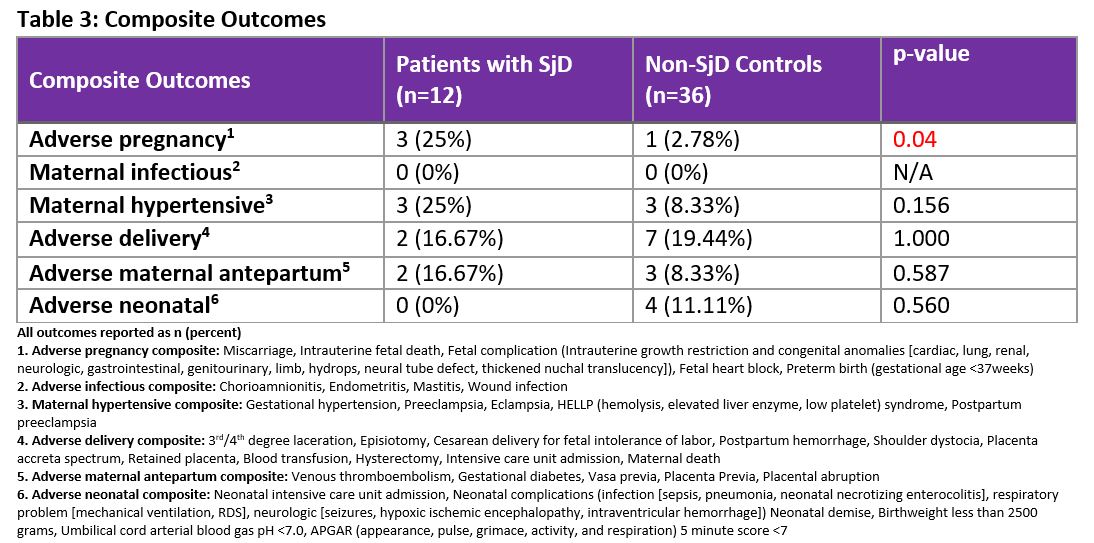
Methods: This was a retrospective cohort study of pregnant patients who had prenatal care and delivered at NYU Langone Hospital-Long Island from 01/2018-12/2022.SjD patients were matched 1:3 with non-SjD controls by gestational age and maternal age. Inclusion criteria for SjD patients were diagnosis by the 2016 ACR/EULAR Criteria or by rheumatologist evaluation, with available pregnancy data. Exclusion criteria for SjD patients were concurrent autoimmune disease (i.e. SLE); antibodies to dsDNA, Smith, or aPL; or unavailable pregnancy records. Controls were excluded if they had major maternal medical comorbidities, major fetal anomalies in pregnancy, prior adverse pregnancy outcome (APO), or delivery elsewhere. Many outcomes of interest are rare, and a composite of grouped outcomes was utilized. All component details of composites are included below (Table 3) and were verified by a MFM specialist. The primary outcome was a composite of APO between the two groups. Secondary analysis included the following composite outcomes: maternal hypertensive, adverse maternal antenatal, adverse delivery, maternal infectious, and adverse neonatal. Statistical analysis of maternal demographics, maternal outcomes, and neonatal outcomes was performed using two sample t-test for continuous variables and Fisher’s exact test for categorical variables, with significance p value of < 0.05.
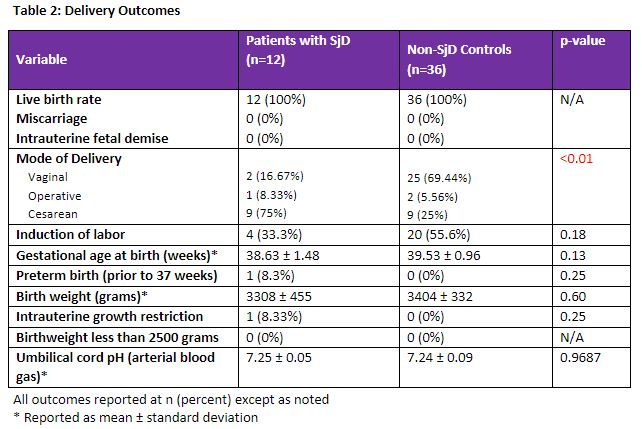
Results: 48 patients were included: 12SjD patients and 36 controls. SjD patients were more likely to be prescribed aspirin (50% vs 5.6%, p = 0.002) and hydroxychloroquine (33.33% vs 0%, p=0.003), while other demographics were comparable (Table 1).The APO composite score was significantly increased in SjD patients (25% vs 2.8% p=0.04) with SjDAPO of 1 preterm birth, 1 fetal growth restriction, and 1 limb anomaly; non-SjD had 1 cardiac anomaly (Table 3).There were no cases of CHB in either group. SjD patients were more likely to be delivered by cesarean delivery(CD) (75% vs 25%, p= 0.004) (Table 2). There were no other significant differences in adverse maternal or neonatal outcomes (Table 2, Table 3).
Conclusion: There was an increased risk of APO in SjD patients compared to controls. No significant difference in neonatal outcomes was noted, adding an important contribution to the limited knowledge of neonatal outcomes in SjD. A significantly increased rate of aspirin use and of CD among patients with SjD was noted and calls for further study. Larger sample size, an interdisciplinary approach with MFM, and the use of rigorous definitions of perinatal outcomes would improve upon our existing knowledge of pregnancy in SjD. Our study suggests that clinicians should consider closer monitoring and early collaboration with MFM specialists for the pregnancies of SjD patients.
To cite this abstract in AMA style:
Tesoriero L, Kidd J, Piccione J, peter I, Akerman M, Carsons S, Rekawek P, Nusbaum J. Adverse Pregnancy Outcomes in Sjogren’s Disease Compared to Controls: An Interdisciplinary Approach with Maternal Fetal Medicine [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/adverse-pregnancy-outcomes-in-sjogrens-disease-compared-to-controls-an-interdisciplinary-approach-with-maternal-fetal-medicine/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/adverse-pregnancy-outcomes-in-sjogrens-disease-compared-to-controls-an-interdisciplinary-approach-with-maternal-fetal-medicine/