Session Information
Date: Sunday, November 7, 2021
Title: Measures & Measurement of Healthcare Quality Poster (0623–0659)
Session Type: Poster Session B
Session Time: 8:30AM-10:30AM
Background/Purpose: Since the first description of polymyalgia rheumatica (PMR) in the early 1950s, the ideal dose and duration of glucocorticoid therapy has varied. In 2015, the American College of Rheumatology (ACR) released guidelines for the management of PMR, and included recommendations on the starting dose of prednisone between 12.5-25mg/day, and suggested tapering strategies to achieve 10mg prednisone/day within 4-8 weeks. In order to evaluate the real world application of these guidelines, we conducted a retrospective analysis of patients diagnosed with PMR and managed by rheumatologists at a single clinic at a tertiary academic center. We further evaluated the screening characteristics for osteoporosis in this population with long term steroid use with a focus on quality improvement.
Methods: Diagnosis codes for PMR were queried for a single rheumatology clinic comprising four physicians and three advanced practice providers. Patients were included if they had an initial diagnosis between January 2015 and June 2020, and had at least four encounters for this diagnosis with a rheumatologist. A retrospective chart review was performed by a single reviewing physician; cases were excluded if they lacked initial laboratory testing for ESR or CRP or had presence of an additional inflammatory rheumatic disease including giant cell arteritis at the time of PMR diagnosis. By consecutive chart review, data was collected on age, race, and sex, ESR and/or CRP. DXA scan performance or physician documentation of known osteoporosis was recorded. Initial prednisone dose, time to taper to 10mg, and total duration of prednisone dose until observation period closed in June 2020 were recorded. Those patients still on prednisone at the end of the study were excluded from analysis for total duration of prednisone used.
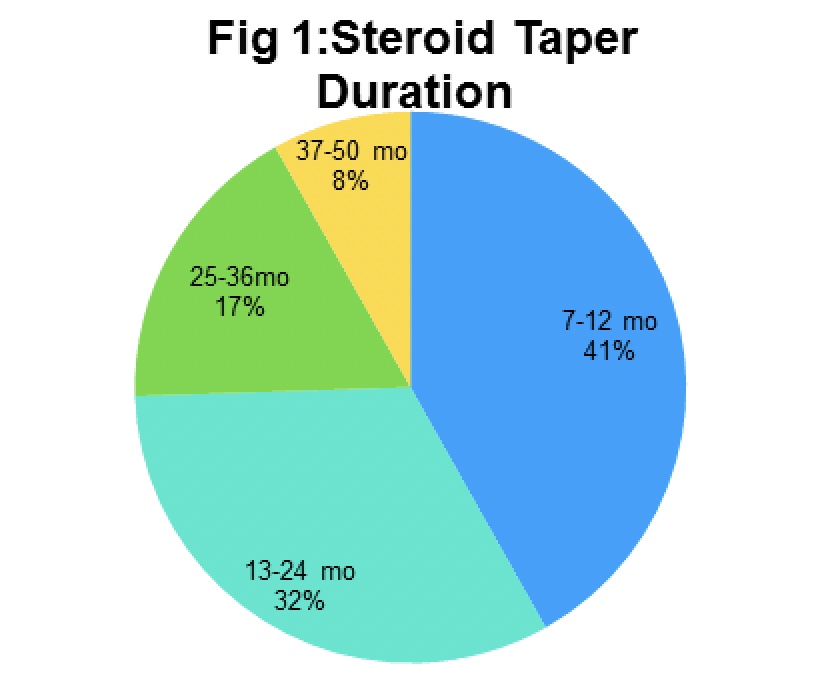
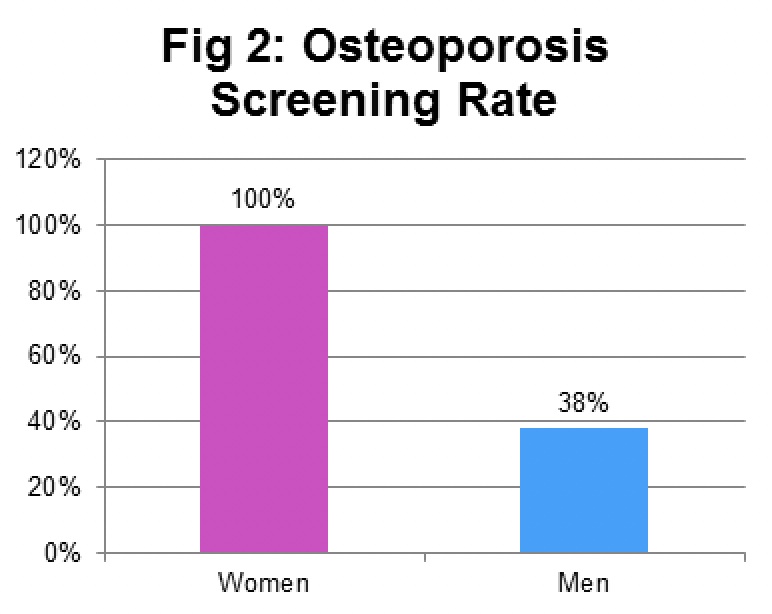
Results: Of the 74 screened patients, 41 patients were enrolled in the cohort for analysis. The cohort consisted of 95% Caucasians, 4% African Americans and 2% Asians; 60% of the enrollees were women (Table 1). The age ranged from 52 to 85 years at the time of diagnosis, with a median of 67 years old. The average starting dose for prednisone was 18mg, within the recommended dose range by the ACR. Only 60% of patients had prednisone tapered to 10mg by week 8. By the end of the observation period, 82% of patients had discontinued glucocorticoids. Of these 34 patients, 41% completed treatment within 7-12 months, 32% within 13-24 months, 17% within 25-36 months and 8% between 37-50 months (Fig 1). Osteoporosis screening was completed in 100% of women but only 38% of men despite the use of prednisone in most cases for longer than two years (Fig 2).
Conclusion: All rheumatology clinicians initiated prednisone treatment within ACR recommended dosing however goal taper prednisone dose of 10mg by 8 weeks was met by only 60% of patients. Male patients had markedly less DXA screening completed, suggesting that this population may be amenable to further quality improvement initiatives to limit steroid toxicity.
To cite this abstract in AMA style:
Parameswaran P, Lucke M. Adherence to the 2015 ACR Guidelines for the Management of Polymyalgia Rheumatica and Screening for Osteoporosis at a Tertiary Care Medical Center [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/adherence-to-the-2015-acr-guidelines-for-the-management-of-polymyalgia-rheumatica-and-screening-for-osteoporosis-at-a-tertiary-care-medical-center/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/adherence-to-the-2015-acr-guidelines-for-the-management-of-polymyalgia-rheumatica-and-screening-for-osteoporosis-at-a-tertiary-care-medical-center/