Session Information
Session Type: Abstract Submissions (ACR)
Background/Purpose Non-adherence to DMARDs is an important indicator for the effectiveness of treatment in early arthritis patients. Reported non-adherence rates differ widely, because studies use different adherence measures. Electronic measurement is considered as a ‘gold standard’, but other measures have other attractive features. This study compared three methods to ascertain how non-adherence should be measured: the Compliance Questionnaire Rheumatology (CQR), the intracellular uptake of methotrexate (MTX) in the form of methotrexate-polyglutamates (MTX-PGs) and Medication Event Monitoring Systems (MEMS).
Methods Adult patients diagnosed with arthritis who started DMARDs were included in a cohort study. MTX-PGs were collected and the CQR was filled out after three and six months of treatment. Non-adherence was continuously measured with MEMS. When there was a discordance between the observed opening and the expected opening of the MEMS cap, this was assigned as a non-adherence event. The CQR and MEMS were compared with Pearson correlations. Sensitivity and specificity of adherence measured with MEMS against a CQR discriminant cut-off score was calculated at three and six months. To assess the influence of adherence measured with MEMS on MTX-PGs, a multivariate linear regression (backward selection) with MTX-PGs as dependent variable and with non-adherence measured with MEMS the 12 weeks before MTX-PG measurement (continuous score), age, gender, time of treatment and dosage as independent variables was performed.
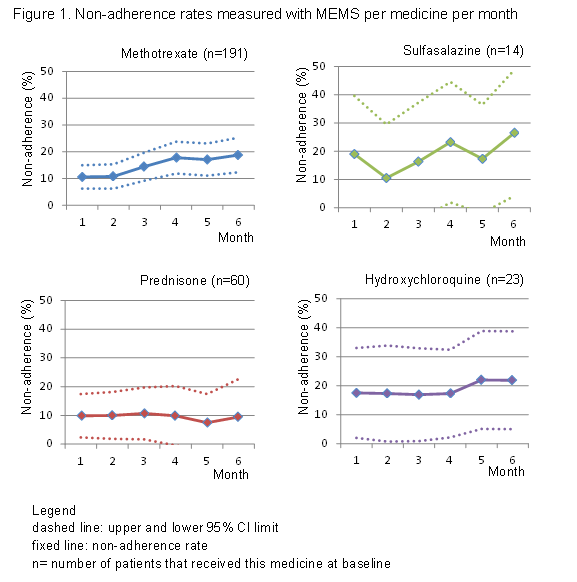
Results Two hundred and one patients entered the study. As measured with MEMS, non-adherence rates varied over time and between different DMARDs (figure 1). For sulfasalazine and hydroxychloroquine, the non-adherence rates were highest. For all medicines, except for prednisone, the non-adherence rate rose over time. The CQR did not correlate with MEMS at any of the time points of therapy. At both time points, the ROC curves showed no discrimination between non-adherence measured with MEMS against the CQR cut-off score. Non-adherence (B 0.548, p=0.035), time of treatment (B 0.947, p=0.006) and age (B 2.052, p<0.000) significantly contributed to MTX-PGs, but only accounted for 18.8% of explained variance.
Conclusion Non-adherence rates for prednisone are lowest and stable. This might be explained by the fact that patients immediately experience the effect of prednisone, and that most patients tapered prednisone. The non-adherence rate for MTX was low, probably because rheumatologists emphasize the necessity of MTX. The CQR is not associated with MEMS, but MTX-PGs are weakly associated with MEMS. This can be due to several reasons, such as individual differences in the uptake of MTX. We have to learn more about the uptake of MTX over time per patient, before we can use MTX-PGs in daily practice as a non-adherence measure.
Disclosure:
A. Pasma,
None;
E. den Boer,
None;
A. van ‘t Spijker,
None;
R. Timman,
None;
J. van Busschbach,
None;
J. M. W. Hazes,
None.
« Back to 2014 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/adherence-to-dmards-in-the-first-six-months-of-treatment-in-early-arthritis-patients-comparing-three-adherence-measures/