Session Information
Date: Saturday, November 16, 2024
Title: Vasculitis – Non-ANCA-Associated & Related Disorders Poster I
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: This systematic literature review on polymyalgia rheumatica (PMR) and PMR with giant cell arteritis (GCA) evaluates existing literature on disease burden, management, and treatment efficacy and safety, identifying knowledge gaps affecting patient care and outcomes. Understanding treatments, diagnostic markers, and quality of life (QOL) can improve the patient journey in PMR and GCA.
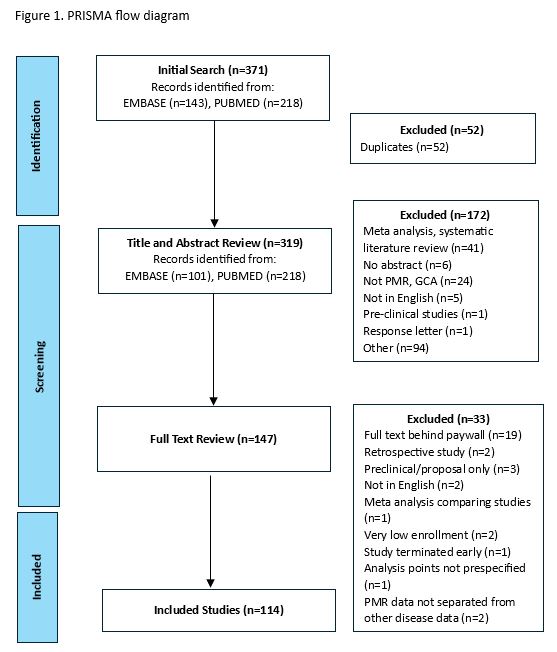
Methods: Using PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines, a systematic search (PubMed, Embase) from November 16, 2023, to January 24, 2024, included key terms like “polymyalgia rheumatica” and “giant cell arteritis” for English language articles published between 1966-2023. Filters applied were “Clinical Trial”, “Meta-Analysis”, “Randomized Controlled Trial”, and “Systematic Review”. The review focused on symptoms, diagnosis, treatment, prognosis, health disparities, and QOL. Abstracts were reviewed by two individuals, with a third adjudicating disagreements. Two reviewers read and summarized 114 full-text articles, assessing quality while noting methods and results. Articles behind paywalls were excluded. An analysis identified commonalities, discrepancies, and research gaps in PMR and PMR with GCA.
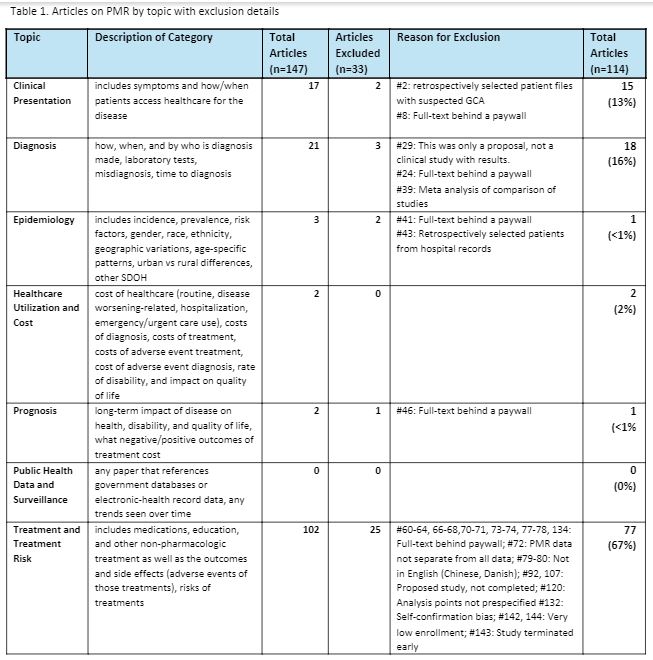
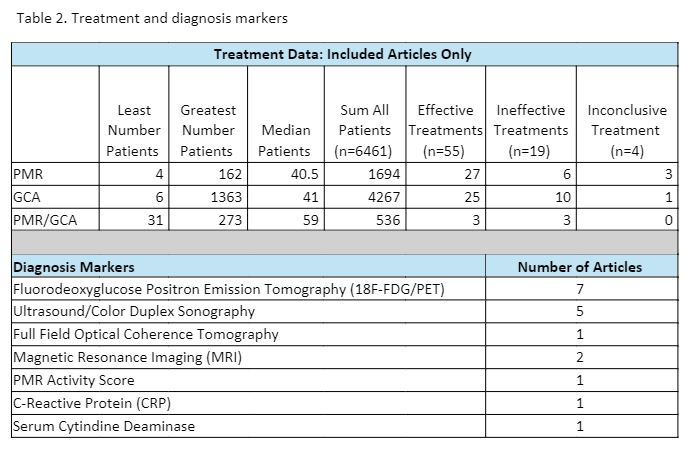
Results: The initial search yielded 371 abstracts; 224 were excluded, and 147 full-text articles were reviewed. Low-quality studies (n=33) were excluded if they did not report results specifically for PMR or GCA, lacked details on identifying or diagnosing patients, or had poorly defined control groups. (Figure 1) The remaining 114 articles were categorized by subtopic (Table 1). Sample sizes ranged from 9 to 1,363 patients, totaling 9,968 patients (PMR: 2,994; GCA: 6,831; PMR and GCA: 143). Less than half (n=52; 45.6%) focused exclusively on PMR. Only two articles (2%) studied patient-reported outcomes (PROs) and QOL. Treatment accounted for 67% of the 114 articles, with diagnosis and clinical presentation comprising 16% and 13%, respectively. Epidemiology, healthcare, prognosis, and public health data made up four percent of all articles. Within treatment, 48% contained data on PMR. Most (83%) treatment articles focused on symptom relief and response; 17% discussed adverse events. Effective treatments (70%) were more common than ineffective (25%) or inconclusive (5%). Main diagnostic biomarkers studied were Fluorodeoxyglucose Positron Emission Tomography (18F-FDG/PET) and Ultrasound/Color Duplex Sonography (Table 2).
Conclusion: The review underscores the need for research addressing gaps in QOL, PROs, diagnosis, and treatment options for PMR. Identifying health disparities is crucial for improving research utility in diverse populations. Low study populations in PMR highlight the need for more research in epidemiology and prognosis. Better diagnostic tools are critical for distinguishing PMR from GCA, enabling prompt and less invasive diagnoses. Monitoring disease activity and PROs, with biomarkers like 18F-FDG/PET, can guide treatment adjustments and improve symptoms. Additional research is vital to enhance patients’ quality of life and longevity. Understanding PMR causes and mechanisms can lead to more effective treatments.
To cite this abstract in AMA style:
Fritz S, Degrassi A, Gavigan K, Hong R, Munoz Perez S, Rivera E, Stone E, Stradford L, Vartak A, Sydor A, Venkatachalam S. Addressing Gaps in Polymyalgia Rheumatica: A Systematic Literature Review [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/addressing-gaps-in-polymyalgia-rheumatica-a-systematic-literature-review/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/addressing-gaps-in-polymyalgia-rheumatica-a-systematic-literature-review/