Session Information
Date: Monday, November 14, 2022
Title: Metabolic and Crystal Arthropathies – Basic and Clinical Science Poster
Session Type: Poster Session D
Session Time: 1:00PM-3:00PM
Background/Purpose: Calcium pyrophosphate deposition disease (CPPD) is a common crystal-induced arthritis characterized by the deposition of calcium pyrophosphate crystals in the articular tissues. Acute CPP crystal arthritis, osteoarthritis with CPPD and chronic CPP crystal inflammatory arthritis are the main manifestations of CPPD. Recent studies have shown that CPPD might be associated with a higher risk of cardiovascular (CV) events related to inflammation. Thus, we aim to examine the outcomes of patients admitted for acute coronary syndrome (ACS) (ST-segment elevation myocardial infarction, non-ST-segment elevation myocardial infarction, unstable angina) with and without CPPD. The primary outcome was to assess the inpatient mortality, hospital length of stay, total hospital charges and inpatient complications.
Methods: We used data from the US National Inpatient Sample (NIS) Database in order to identify patients who were admitted for ACS between 2006 and 2019. The ICD-9 and -10 codes were used to determine the patients with ACS-related hospitalizations and of those, we classified two groups of patients: (i) those with ICD-9 and -10 codes defining CPPD and (ii) those without any CPPD code. Data collection included patient demographics and comorbidities. Outcomes were in-hospital mortality, length of hospital stay, hospital charges, and in-hospital complications. Associations between CPPD and specific morbidity were evaluated with chi-square tests. T-tests were used for continuous variables. We have also presented odds ratio (OR) along with 95% confidence intervals (CI) for the outcomes of interest.
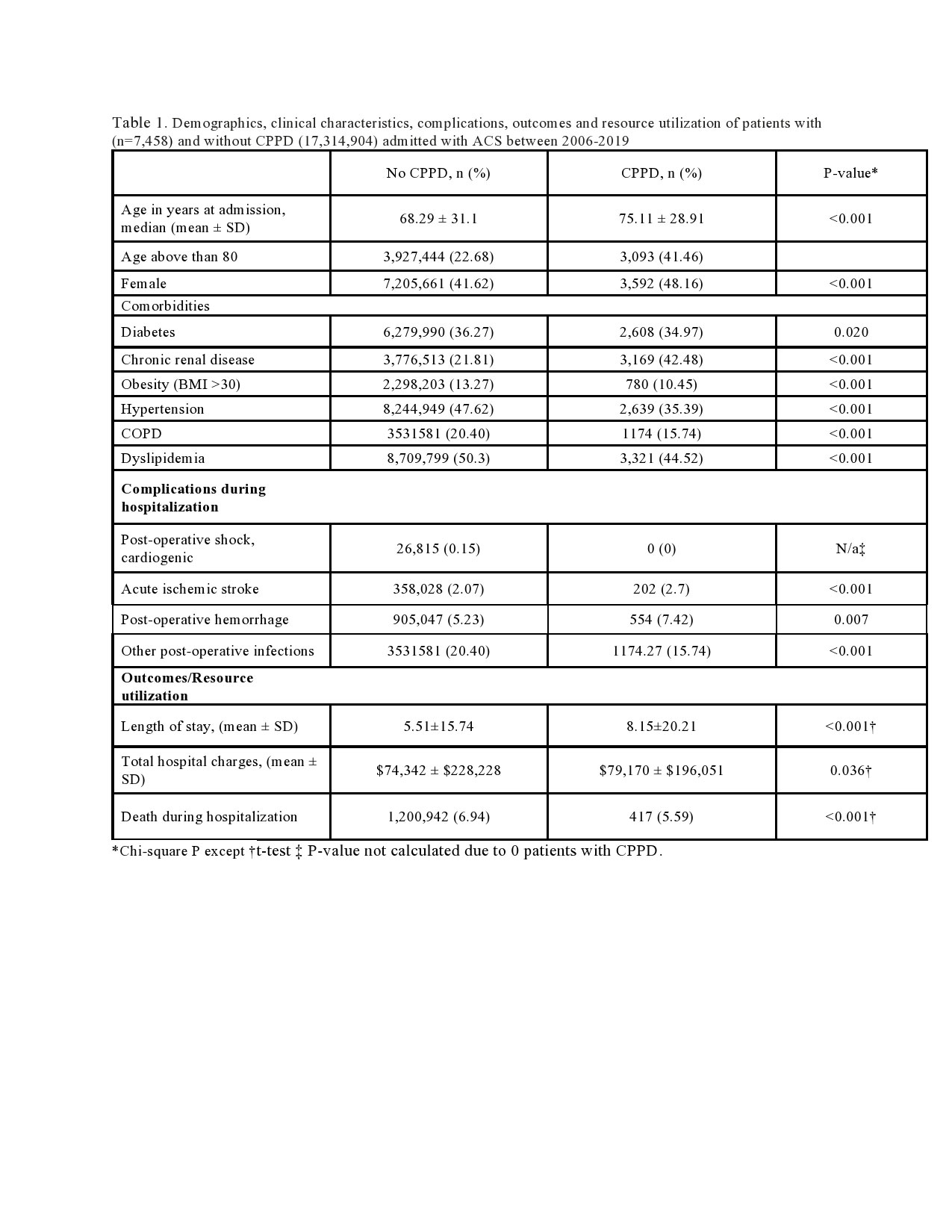
Results: A total of 17,322,362 (adjusted for sampling weight) patients were admitted for ACS between 2006 and 2019. Among them, 7,458 had CPPD, with a mean age of 75 years and 48% were females (Table 1). CPPD patients were more likely to be older (mean age 75 vs 68 years; p< 0.001) compared to non-CPPD patients. Among the comorbidities, chronic kidney disease was more frequently observed in CPPD patients. Regarding the inpatient complications, acute ischemic stroke and post-procedural hemorrhage myocardial infarction were more frequently seen in the CPPD patients. Interestingly, the in-hospital mortality was lower in the CPPD patients than the non-CPPD patients (5.5% vs 6.9 %, p < 0.001) (OR 0.79, CI 95% 0.71-0.87). ACS in CPPD patients was associated with a longer mean length of stay than those without CPPD (8.15 vs 5.5 days; p < 0.001; OR 3, CI 95% 2.8-3.1). In addition, mean total charges were higher in the CPPD group ($79,170 vs $74,342; p=0.036; OR 1.06, CI 95% 1.02-1.11).
Conclusion: ACS in CPPD patients is associated with higher healthcare utilization, including cost and length of hospital stay, and lower in-hospital mortality than non-CPPD patients.
To cite this abstract in AMA style:
Parperis K, Bhattarai B. Acute Coronary Syndrome in Calcium Pyrophosphate Deposition Disease Patients: A Cross-sectional Study from the National Inpatient Sample [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/acute-coronary-syndrome-in-calcium-pyrophosphate-deposition-disease-patients-a-cross-sectional-study-from-the-national-inpatient-sample/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/acute-coronary-syndrome-in-calcium-pyrophosphate-deposition-disease-patients-a-cross-sectional-study-from-the-national-inpatient-sample/