Session Information
Session Type: ACR Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: The 2015 Workforce Study (WFS) sought to expand our current understanding of the rheumatology workforce utilizing an integrated, patient-centered approach to workforce modeling. Primary data from rheumatology patientsÕ perspectives was collected to help inform access to care issues.
Methods: The 2015 WFS used several primary and secondary data sources, including the ACR member database, state licensure registries, 2005 ACR workforce study results, professional organization information and peer-reviewed literature. These data were supplemented with survey data collected from adult, young adult and parents of pediatric rheumatology patients with assistance from the Arthritis Foundation. Face, content, and criterion validity was established through a team of rheumatology/survey research professionals. Overall internal reliability was established (Adult Survey: r=0.82; Pediatric/Young Adult Survey: r=0.85).
Results: Respondents were from 49 states representing all major regions of the U.S. (Adult=564; Young Adult=76; Pediatric=292); not all respondents answered every item. A majority self-identified as having private insurance. Approximately 48% (n=274) of adult, 55% (n=160) pediatric, and 40% (n=30) young adult patients were diagnosed by a rheumatologist, with the remainder diagnosed by their PCP or a non-rheumatology specialist. While a majority were able to see a rheumatologist within 3 months of onset of symptoms, there were still 30% (n=155) of adults, 26% (n=77) pediatric, and 26% (n=20) young adults who had over a 4 month wait to see a rheumatologist. When asked about the ease of obtaining regular follow-up appointments, 78% (n=430) of adults reported they were able to make routine appointments within the timeframe recommended by their rheumatologist, whereas only 57% (n=193) pediatric and young adult patients were able to do so. 50% (n=283) adults, 57% (n=165) pediatric, and 61% (n=46) young adults indicated it was somewhat to very difficult to make an urgent care appointment. 67% adults (n=372) adults and 55% (n=202) pediatric/young adults went to their PCP for urgent care if they could not see their rheumatologist. 13% (n=72) adults, 7% (n=17) young adults, and 57% (n=166) pediatric patients indicated there was not a rheumatologist within 25 miles from their home. 31% (n=90) pediatric patients reported having to travel more than 2 hours. In addition to travel time, respondents reported major travel costs related to fuel and missing work (Table 1).
Conclusion: Access to care is a substantial issue for patients, with major potential impact on quality and outcomes. There are substantial direct and indirect costs for patients in obtaining rheumatologic care, especially for pediatric patients. These data realistically enhance our understanding of access to care challenges for rheumatology patients. 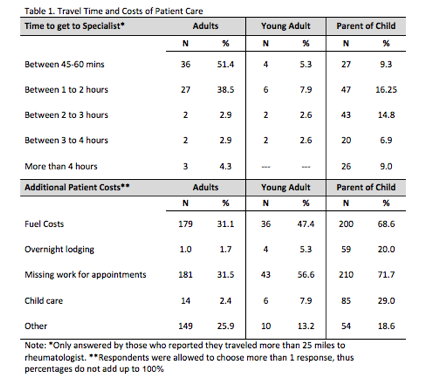
To cite this abstract in AMA style:
Monrad S, Imundo L, Battafarano D, Ditmyer M. Access to Care: The Patient Perspective from the 2015 ACR/ARHP Workforce Study [abstract]. Arthritis Rheumatol. 2016; 68 (suppl 10). https://acrabstracts.org/abstract/access-to-care-the-patient-perspective-from-the-2015-acrarhp-workforce-study/. Accessed .« Back to 2016 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/access-to-care-the-patient-perspective-from-the-2015-acrarhp-workforce-study/
