Session Information
Date: Wednesday, November 13, 2019
Title: 6W010: Pediatric Rheumatology – Clinical III: Juvenile SLE & Dermatomyositis (2864–2869)
Session Type: ACR Abstract Session
Session Time: 9:00AM-10:30AM
Background/Purpose: Factors associated with diagnostic delay in Juvenile Dermatomyositis (JDM) are not known. We hypothesized that limited access to pediatric rheumatologists can lead to delay in the diagnosis of JDM and worse outcomes. We investigated demographic factors, including access to care, associated with diagnostic delays and clinical outcomes of subjects with JDM in the Childhood Arthritis and Rheumatology Research Alliance (CARRA) Legacy Registry.
Methods: This was a cross-sectional study of JDM subjects enrolled in the CARRA Legacy Registry from 2010-2015. We used two measures of access to care: distance to care, calculated as miles by driving from subject zip code to treating rheumatology center using the R package “gmapsdistance”, and state density of pediatric rheumatologists calculated as child population divided by number of pediatric rheumatologists. An ordered generalized additive model (GAM) was used to determine the association these two predictors, included as smoothed terms, and diagnostic delay adjusting for age, sex, income, and race. Delay was categorized as early (< 30 days), typical (1-3 mos), moderate (3-12 mos) and severe ( >12 mos). The association between access to care and patient outcomes, including physician and parent global scores, childhood HAQ, and ACR functional class, was also assessed.
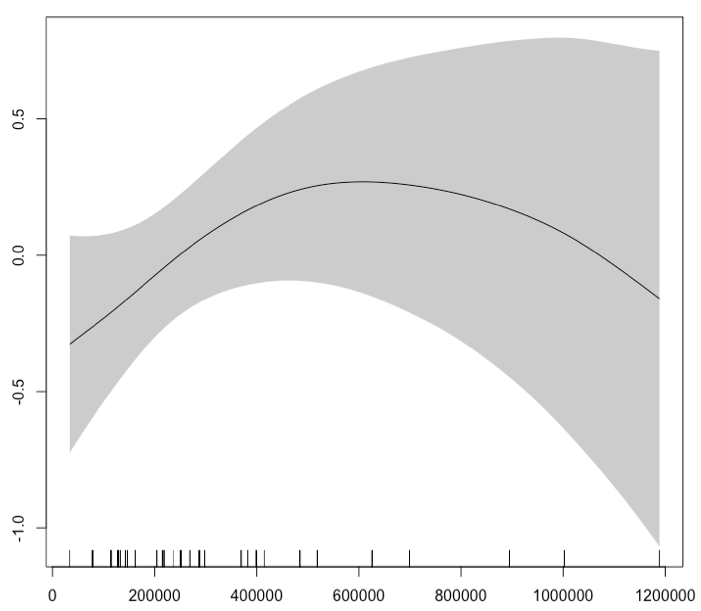
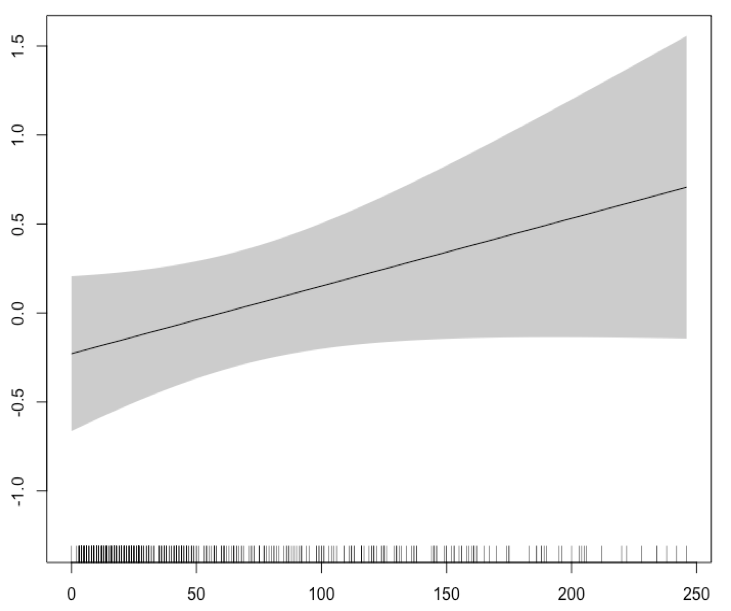
Results: A total of 464 JDM subjects were included in the analysis. The median time to diagnosis was 3.1 months (IQR 1.4-7.0). Moderate to severe diagnostic delay was found in nearly 52% of subjects. The median distance to care was 37.5 miles (IQR 17.0-90.3). The median density of children per pediatric rheumatologist was approximately 250,000 (IQR 147,000-399,000). In an ordered GAM, there was a modest association between greater delay in states with more children per pediatric rheumatologist (AIC decrease of 1.4, p = 0.060, Fig 1), a trend that was observed up to 500,000 children per rheumatologist, after which the confidence intervals widened due to few observations in very underserved states. Younger age at JDM onset was associated with diagnostic delay (OR 0.94 per year increase, p = 0.01), while having a household income >$150,000 compared to < $25,000 was protective (OR 0.47, p = 0.04). Non-black minority race compared to white race was also protective against delay (OR 0.43, p = 0.01). There was a modest trend toward having more functional limitation as measured by current ACR class of 2 or greater with increasing distance to care (AIC decrease of 0.9, p = 0.08, Fig 2).
Conclusion: In the CARRA Legacy Registry, we found moderate to severe diagnostic delays in the majority of subjects with JDM. Our data suggests that access to care, measured as density of rheumatologist by state, is an important factor associated with delay in care but also highlights other contributing demographic factors, including younger age at disease onset and poverty. We also found a trend towards more functional limitation in patients with increasing distance to care. In addition to increasing the pediatric rheumatology workforce, efforts to increase awareness of rare conditions like JDM among general practitioners and subspecialists may help shorten referral time to pediatric rheumatologists and improve outcome in patients with JDM.
To cite this abstract in AMA style:
Neely J, Kim S, Sturrock H, Shalen J. Access to Care and Diagnostic Delays in Juvenile Dermatomyositis [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/access-to-care-and-diagnostic-delays-in-juvenile-dermatomyositis/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/access-to-care-and-diagnostic-delays-in-juvenile-dermatomyositis/