Session Information
Session Type: ACR Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Ten years have elapsed since the last ACR workforce study (WFS), and it is anticipated that rheumatologists will face many challenges to train and sustain a workforce of rheumatology specialists that will meet future needs. Analyzing the current workplace and identifying barriers to practice may help identify strategies and solutions.
Methods: As part of the WFS, a web-based survey was administered to the ACR membership, targeting clinically active practitioners. Survey responses were analyzed to compare demographics, practice patterns, retirement planning, and barriers to practice between rheumatologists working in academic work settings vs. those in non-academic work settings. Qualitative data was gathered regarding barriers to practice and assessed to identify common themes.
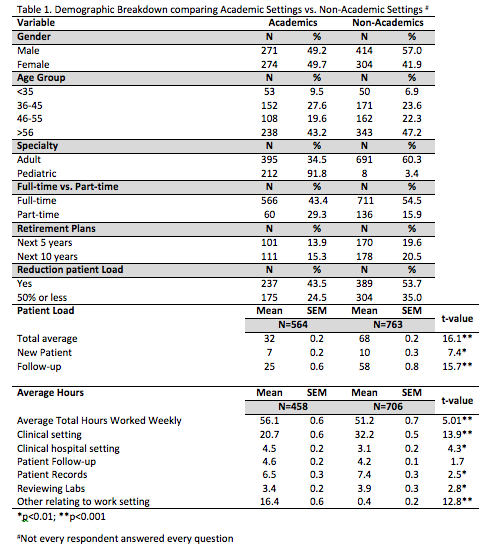
Results: There were a total of 1996 completed survey responses (31.5% response rate: 1996/6342) 1,578 of which provided information about practice setting and were included in the analysis; not every respondent answered every question. 54.5% (n=868) of respondents self-reported their primary work setting as non-academic (including solo practice, single- and multi-specialty, and government) vs. 45.5% (n=726) who reported working in academic settings. Demographics are listed in Table 1. Non-academics reported working slightly fewer hours per week than academics, but spent 50% more time seeing patients, and saw more than twice as many patients each week. Weak correlations were found in average reported work hours per week and patient workload (r=0.227; p<0.01) between academics and non-academics. 40% (n=348) of non-academic practitioners anticipate retiring in the next 10 years, compared with 29% (n=212) in academic settings. Almost 60% (n=391) of non-academic practitioners plan to reduce their patient load in the next ten years by up to 50%, compared to 40% (n=262) of academicians.
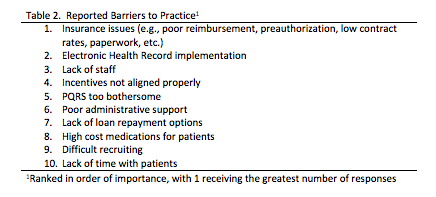
Table 2 lists the top 10 barriers to practice reported by respondents. Insurance issues and electronic health records (EHR) were the top two (2) barriers to practice reported by both those working in non-academic and academic settings. Two common areas of dissatisfaction were reimbursement rates (n=476; 29.8%) and requirements for EHR (n=457; 28.6%).
Conclusion: Despite a number of differences between current practitioners in academic vs non academics, rheumatologists identify common and pervasive barriers to practice regardless of practice setting. Advocacy efforts focusing on reimbursement levels and EHR implementation/use should be a high priority to help support the existing and future workforce.
To cite this abstract in AMA style:
Monrad S, Battafarano D, Ditmyer M. Academic and Non-Academic Rheumatology: Practice Trends and Common Barriers to Practice from the 2015 ACR/ARHP Workforce Study Survey [abstract]. Arthritis Rheumatol. 2016; 68 (suppl 10). https://acrabstracts.org/abstract/academic-and-non-academic-rheumatology-practice-trends-and-common-barriers-to-practice-from-the-2015-acrarhp-workforce-study-survey/. Accessed .« Back to 2016 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/academic-and-non-academic-rheumatology-practice-trends-and-common-barriers-to-practice-from-the-2015-acrarhp-workforce-study-survey/