Session Information
Date: Sunday, October 21, 2018
Title: Pediatric Rheumatology – Clinical Poster I: Lupus, Sjögren’s Disease, and Myositis
Session Type: ACR Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: SLE is a chronic, multisystem autoimmune condition with multiple comorbidities due to inflammation and treatment, including metabolic syndrome, poor cardiac outcome, and poor quality of life. Obesity is more prevalent in children with jSLE compared to the general population. Obesity induces inflammation and independently contributes to lower functional status. Corticosteroid (CS) use is associated with weight gain. Obesity is also more prevalent in youths of lower socioeconomic status (SES). This study aims to retrospectively study weight change in an inception cohort of jSLE and potential contributors.
Methods: A retrospective chart review of jSLE was conducted at a single medical center. Inclusion criteria were an ICD-9 or ICD-10 diagnosis of jSLE prior to 18 years of age and multiple visits in the first year of jSLE. Baseline data included demographics and serologies. Variables collected from each visit included: time from diagnosis; age; weight, height, and BMI with percentiles and Z-scores; documentation of fatigue, gastrointestinal, psychiatric, or musculoskeletal symptoms; albumin; SLEDAI; and current medications with CS dose in mg/kg of prednisone. A mixed effect model was used to determine associations between BMI change and individual factors.
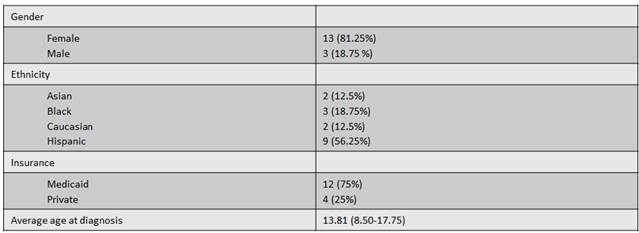
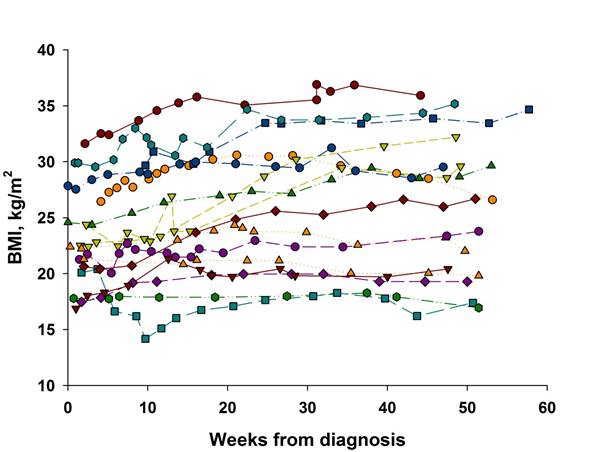
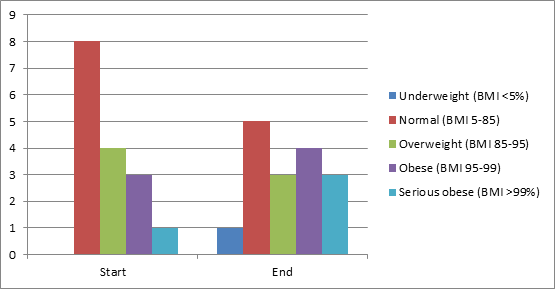
Results: Interim analysis included 16 patients, who were predominantly female, Hispanic, and on Medicaid (Table 1). Average age of diagnosis was 13.81 years. There was an average 0.064±0.007 kg/m2 increase in BMI per week (p<0.001). Clinically, the number of obese and seriously obese patients increased from 25% to 43.75%. CS dose and SLEDAI were inversely associated with BMI (p<0.001, p=0.017). There was a trend towards association between higher BMI and fatigue (p=0.168), gastrointestinal (p=0.074), psychiatric (p=0.801), and no musculoskeletal symptoms (p=0.403).
Conclusion: There is a statistically significant trend towards increasing weight in the first year of jSLE and an increased rate of obesity. Increasing BMI was significantly associated with lower CS dose and SLEDAI and was associated with a more positive review of symptoms. Future study will expand this cohort, examine the impact of growth, and direct prospective studies.
Table 1. Patient characteristics.
Figure 1. Change in patient BMI.
Figure 2. Change in BMI status.
To cite this abstract in AMA style:
Treemarcki E, Szymonifka J, Adams A, Pan N, Taber S, Onel K. A Weighty Diagnosis: Weight Change and Risk Factors in Early Juvenile Systemic Lupus Erythematosus [abstract]. Arthritis Rheumatol. 2018; 70 (suppl 9). https://acrabstracts.org/abstract/a-weighty-diagnosis-weight-change-and-risk-factors-in-early-juvenile-systemic-lupus-erythematosus/. Accessed .« Back to 2018 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/a-weighty-diagnosis-weight-change-and-risk-factors-in-early-juvenile-systemic-lupus-erythematosus/