Session Information
The 2020 Pediatric Rheumatology Symposium, originally scheduled for April 29 – May 2, was postponed due to COVID-19; therefore, abstracts were not presented as scheduled.
Date: Saturday, May 2, 2020
Title: Poster Session 3
Session Type: ACR Abstract Session
Session Time: 4:15PM-5:15PM
Background/Purpose: Chronic anterior uveitis is a sight-threatening complication of juvenile idiopathic arthritis (JIA). Prompt treatment to prevent complications requires regular screening and detection of uveitis before vision loss is clinically apparent. Rates of adherence to eye screening recommendations in patients with JIA are unknown. The authors’ experience suggests that JIA patients receive variable education about uveitis and may have low understanding of uveitis complications, and timing and required components of screening exams. This survey assessed JIA patient and parent knowledge about uveitis complications and screening recommendations.
Methods: A 21-item survey was developed, comprised of six demographic questions, six arthritis/uveitis history questions, and nine uveitis knowledge questions. The survey was administered to adolescents age 14 and older with JIA and parents of patients with JIA. Respondents were recruited from three geographically diverse pediatric rheumatology practices and online through the Patients, Advocates, and Rheumatology Teams Network for Research and Service (PARTNERS) network. An overall knowledge score was calculated as a composite of the nine individual knowledge questions (Table 1).
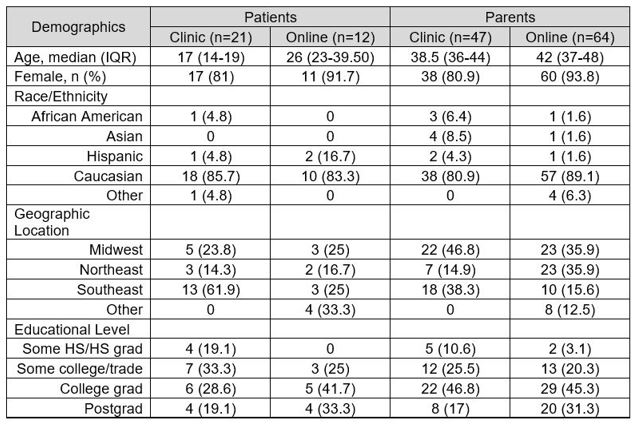
Results: 33 patients and 111 parents completed the survey in clinic or online (Table 2). Respondents were predominantly Caucasian with a relatively high educational level. Overall, 22.5% had a personal history of uveitis. 89.5% of participants had heard of uveitis, though knowledge of potential uveitis complications and screening recommendations were lower in all groups (Table 3). The mean composite score was 6.46 (sd 2.6) out of 9. Parent respondents who completed the survey online through PARTNERS had a higher composite score (7.22) than parents completing the survey in clinic or patients completing the survey through PARTNERS or in clinic (5.96, 5.92, 5.57, respectively, p=0.02). Patients with a history of uveitis had higher composite knowledge scores than those without a uveitis history (8.3 vs 5, p=0.01). The same was true for parents who reported a history of uveitis in their child (8.6 vs 6.3, p< 0.01). Parents who reported that their rheumatologist reminded them about eye exams at every visit had higher knowledge of the risk of blindness (p=0.03), the risk for uveitis when arthritis is controlled (p=0.05), the need for ongoing eye exams when off medications (p=0.01), and had a higher overall score (p=0.02) than those who were reminded at some visits or not at all.
Conclusion: Adolescents with JIA and their parents report variable levels of knowledge regarding uveitis complications and recommended screening. Frequent discussion between the rheumatology provider and family about uveitis screening was significantly related to having more uveitis knowledge. As gaps in knowledge may impact motivation to adhere to screening intervals, incorporating detailed and frequent education about uveitis into rheumatology clinic appointments is essential to ensuring good visual outcomes.
Acknowledgements
The authors would like to acknowledge PARTNERS and the Arthritis Foundation for their support of this study.
To cite this abstract in AMA style:
Cooper A, Flanagan E, Ronis T, Goldberg B, Sherman A, Smith C, Holland G. A Survey of Uveitis Knowledge Among Juvenile Arthritis Patients and Parents [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 4). https://acrabstracts.org/abstract/a-survey-of-uveitis-knowledge-among-juvenile-arthritis-patients-and-parents/. Accessed .« Back to 2020 Pediatric Rheumatology Symposium
ACR Meeting Abstracts - https://acrabstracts.org/abstract/a-survey-of-uveitis-knowledge-among-juvenile-arthritis-patients-and-parents/