Session Information
Session Type: Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: There is a lack of guidance surrounding integration of Advanced Practice Providers (APPs) into specialty practices utilizing interprofessional Models of Care (MoC). Due to current and projected workforce shortages combined with rising patient need in the field of Rheumatology, multiple methods were utilized to engage both APP and physician perspectives to develop a MoC specific to an academic Rheumatology practice. Initial goals included understanding the current and desired MoC, as well as integration of APPs into optimized models.
Methods: Utilizing a mixed methods sequential-exploratory design through a quality improvement lens, a blueprint for a MOC re-design was developed and will be presented here. Quality Improvement (QI) strategies planned: 1. Needs assessment 2. Baseline data collection 3. Dissemination 4. Team building 5. Implementation 6. Evaluation with ongoing improvements as needed (Figure 1). Phases one through four were completed as part of this project with divisional consideration for implementation of phases five and six in the future.
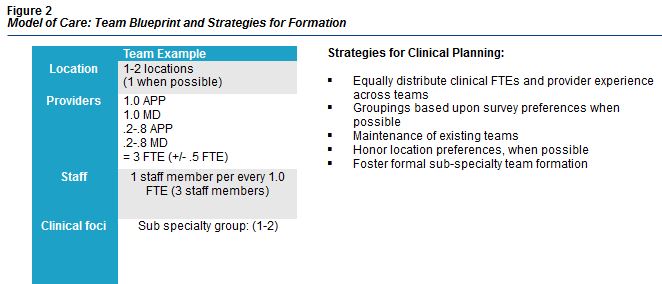
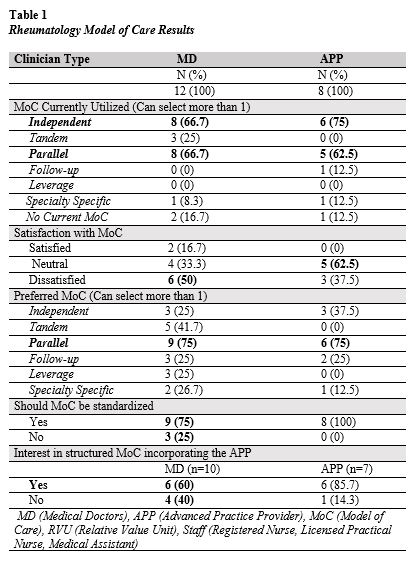
Results: In the needs assessment phase, we interviewed key stakeholders (divisional leadership) to develop shared goals for the optimal MoC. These goals included quality of patient care, access, and addressing barriers at the patient, physician, APP, environmental, and organizational levels. In the next phase, data collection, we distributed a survey to 12 physicians and 8 APPs in our practice addressing eleven domains: 1. Models of Care 2. Physician 3. Appropriateness of an APP to see 17 common Rheumatological diagnoses as a new or return visit 4. Logistical Considerations 5. Staff Utilization 6. Provider Satisfaction 7. Telehealth Preferences 8. Patient Impact 9. Burnout Inventory 10. Work Life Balance and 11. Joy in Work. During phase three, key findings were communicated with divisional leadership and then with clinicians and staff followed by an iterative process for team building and design in phase four. Surveys showed low satisfaction with the current MoC. These findings suggest that the APP is being utilized in variable MoC and that many physicians are dissatisfied with current MoC. Additionally, strong preferences for parallel and independent practice, standardization of MoC, and a formal structure that integrates the APP was preferred by both APPs and Physicians (Table 1). The top two clinician foci for the MoC included quality of care and prevention of burnout. Clinicians agreed that the main barriers to implementing a MoC were a lack of a well-defined and documented MoC, clinic space and communication. Based upon these findings, a proposed team-based MoC was developed (Figure 2).
Conclusion: Using a mixed methods QI approach is effective to elicit clinical needs and barriers with significant clinician buy-in. Improved understanding of clinicians’ desired MoC and what this MoC should focus on impacts team-based structures, for which the APP is a critical component. As the role of the APP is predominantly geared towards the clinical mission, improving full scope integration of the APP via MoC re-design in specialty practices, including Rheumatology, is pivotal to improve the quality of patient care and access.
To cite this abstract in AMA style:
Carnago L, Holbrook K, Leverenz D, Rivera N, Dimsdale A. A Rheumatology Model of Care Re-design: Integrating the Advanced Practice Provider [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/a-rheumatology-model-of-care-re-design-integrating-the-advanced-practice-provider/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/a-rheumatology-model-of-care-re-design-integrating-the-advanced-practice-provider/