Session Information
Title: Pediatric Rheumatology - Clinical and Therapeutic Aspects: Pediatric Systemic Lupus Erythematosus
Session Type: Abstract Submissions (ACR)
Background/Purpose Lupus Nephritis (LN) occurs in up to 80% of childhood-onset Systemic Lupus Erythematosus (cSLE) and it has a worse prognosis than adults. The current gold standard for diagnosing LN and assessing its activity is a kidney biopsy interpreted using the International Societies for Nephrology & Renal Pathology (ISN/RPS) classification. Kidney biopsies are invasive and too costly to assess the course of LN. The objective of this study is to develop and initially validate for Children a Renal Activity Index (C-RAI) to non-invasively monitor LN activity, considering both traditional measures of LN (LN-TM) and recently discovered renal biomarkers (RBM).
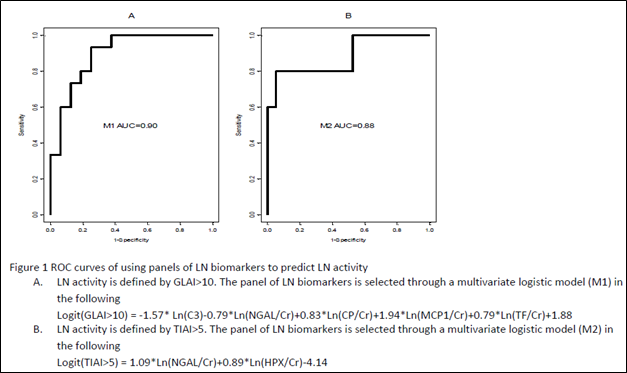
Methods In this ongoing prospective study, 83 children with LN were studied at the time of the kidney biopsy; LN-TM [GFR, complements, anti-dsDNA antibodies, urinary protein/creatinine ratio], clinical indices [Systemic Lupus International Collaborating Clinics Renal Activity Score (SLICC-RAS), renal domain score of BILAG (BILAG-R) and SLEDAI (SLEDAI-R)] were all obtained, and the RBM (Table 1) were measured. Histological findings were rated by a single nephropathologist who provided ISN/RPS class, NIH Glomerular Activity Index (GLAI; range 0-24) and Tubulointerstitial Activity Index (TIAI; range = 0-21) scores (Criterion Standards). Prior to statistical analysis, RBM levels were normalized by urine creatinine and logarithmically transformed. LN-TM, RBM and clinical indices that showed significance in univariate analysis at a p-value<0.10 were considered in stepwise multivariate logistical regression models as C-RAI candidate predictors, using the GLAI and TIAI as dependent variable (outcome). The accuracy of the C-RAI of predicting and discriminating LN activity was assessed by receiver-operating characteristic curve (ROC) analysis.
Results Means and percentages of the values of LN-TM, clinical indices and RBM levels are summarized inTable1. Based on multivariate logistical regression modeling, histological activity measurement does not necessitate consideration of clinical indices but rather select LN-TM and RBM. Levels of C3, NGAL, CP, MCP1 and TF were found to be candidate C-RAI’s for predicting high LN activity (GLAI>10) with outstanding accuracy [area under the ROC curve (AUC) = 0.9]. NGAL and HPX were excellent predictors of high interstitial inflammation with active LN (TIAI > 5; AUC = 0.88) (Figure1).
Conclusion C3 level, NGAL, CP, MCP1, TF, and HPX are good potential components for C-RAI to measure histological LN activity in the glomeruli and interstitium. Confirmation in a larger data set is required.
|
Table1 Comparisons of LN biomarkers between NIH GLAI and TIAI classes |
||||||||
|
LN biomarkers |
GLAI Score |
TIAI Score |
||||||
|
≤ 10 |
> 10 |
p |
≤ 5 |
> 5 |
p |
|||
|
SLEDAI-R* |
7.45 (6.06, 8.84) |
11.93 (10.15, 13.70) |
0.000 |
8.20 (6.75, 9.64) |
11.43 (8.96, 13.90) |
0.031 |
||
|
BILAG-R* |
10.37 (9.52, 11.23) |
11.56 (10.48, 12.63) |
0.096 |
10.93 (10.02, 11.83) |
10.86 (9.33, 12.38) |
0.940 |
||
|
SLICC-RAS* |
4.38 (2.75, 6.02) |
7.58 (5.57, 9.58) |
0.019 |
5.20 (3.47, 6.92) |
5.92 (2.86, 8.98) |
0.686 |
||
|
Protein/ Cr ratio* |
1.79 (1.20, 2.67) |
2.85 (1.74, 4.67) |
0.156 |
1.98 (1.31, 2.97) |
2.67 (1.31, 5.42) |
0.474 |
||
|
Urine Protein* |
185.74 (101.62, 339.49) |
423.73 (206.08, 871.27) |
0.106 |
185.43 (107.15, 320.90) |
541.85 (221.27, 1,326.88) |
0.076 |
||
|
GFR* |
115.07 (97.38, 135.97) |
75.53 (61.04, 93.47) |
0.003 |
108.48 (94.32, 124.78) |
69.64 (54.81, 88.48) |
0.003 |
||
|
Serum Cr* |
0.63 (0.55, 0.74) |
0.99 (0.82, 1.20) |
0.001 |
0.66 (0.58, 0.76) |
1.06 (0.85, 1.33) |
0.001 |
||
|
C3 level* |
64.28 (53.79, 76.82) |
41.94 (33.44, 52.60) |
0.005 |
53.31 (43.72, 65.01) |
52.35 (37.43, 73.22) |
0.928 |
||
|
C3 (Low)** |
47.62% |
15.38% |
0.010 |
30.00% |
28.57% |
0.920 |
||
|
C4 level* |
9.95 (7.92, 12.50) |
6.35 (4.80, 8.41) |
0.018 |
7.63 (6.04, 9.64) |
7.67 (5.17, 11.39) |
0.982 |
||
|
C4 (Low)** |
30.95% |
14.81% |
0.137 |
25.00% |
21.43% |
0.788 |
||
|
DSDNA (Positive)** |
16.67% |
8.00% |
0.334 |
11.43% |
9.09% |
0.828 |
||
|
NGAL |
0.25 (0.15, 0.43) |
0.65 (0.36, 1.17) |
0.027 |
0.30 (0.17, 0.50) |
0.93 (0.35, 2.42) |
0.052 |
||
|
CP |
118 (64, 215) |
334 (173, 645) |
0.028 |
199 (108, 367) |
266 (87, 813) |
0.661 |
||
|
MCP1 |
5.88 (3.85, 8.97) |
24.04 (15.16, 38.10) |
0.000 |
8.99 (5.42, 14.91) |
30.25 (12.01, 76.23) |
0.033 |
||
|
AGP |
561 (232, 1,359) |
1,101 (397, 3,057) |
0.337 |
593 (232, 1,516) |
3,752 (402, 35,064) |
0.153 |
||
|
TGFB* |
0.42 (0.26, 0.69) |
1.27 (0.86, 1.86) |
0.004 |
0.73 (0.46, 1.17) |
1.56 (0.83, 2.91) |
0.083 |
||
|
ADI |
0.09 (0.03, 0.23) |
0.51 (0.17, 1.49) |
0.023 |
0.11 (0.04, 0.28) |
1.35 (0.22, 8.33) |
0.024 |
||
|
HEPCIDIN |
0.55 (0.26, 1.15) |
0.66 (0.29, 1.47) |
0.753 |
0.56 (0.26, 1.21) |
0.70 (0.15, 3.28) |
0.802 |
||
|
LPGDS |
2.71 (1.56, 4.70) |
5.74 (3.15, 10.48) |
0.080 |
3.24 (1.84, 5.69) |
8.04 (2.87, 22.51) |
0.141 |
||
|
TF |
0.09 (0.05, 0.15) |
0.17 (0.10, 0.31) |
0.083 |
0.11 (0.07, 0.19) |
0.18 (0.07, 0.45) |
0.395 |
||
|
VDBP |
5.43 (2.26, 13.07) |
6.19 (2.38, 16.14) |
0.844 |
3.95 (1.72, 9.08) |
30.18 (6.62, 137.64) |
0.030 |
||
|
HPX |
17.15 (9.01, 32.65) |
35.64 (17.97, 70.70) |
0.138 |
17.52 (9.76, 31.45) |
109.68 (35.05, 343.16) |
0.010 |
||
|
*: Values in the cells are mean (95% CI); NGAL: neutrophil gelatinase associated lipocalin, MCP1: monocyte chemoattractant protein-1, CP: ceruloplasmin, AGP: alpha1-acid glycoprotein, TF: transferrin, LPDGS: lipocalin-like prostaglandin-D Synthase, ADI: adiponectin, HPX: hemopexin, TGFB: TGF-beta, , VDBP: vitamin D binding protein. |
||||||||
Disclosure:
K. Abulaban,
None;
M. Bennett,
None;
M. Klein-Gitelman,
None;
S. P. Ardoin,
None;
K. A. Rouster-Stevens,
None;
L. B. Tucker,
None;
K. Wiley,
None;
S. Nelson,
None;
K. Onel,
None;
N. G. Singer,
None;
K. M. O’Neil,
None;
E. Brooks,
None;
B. A. Eberhard,
None;
L. K. Jung,
None;
L. F. Imundo,
None;
T. Wright,
None;
D. Witte,
None;
J. Ying,
None;
P. Devarajan,
None;
H. I. Brunner,
TMA and NIEHS,
9.
« Back to 2014 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/a-renal-activity-index-may-predict-histological-activity-in-lupus-nephritis-in-children/