Session Information
Session Type: Abstract Session
Session Time: 1:00PM-2:30PM
Background/Purpose: Rheumatoid Arthritis (RA) and Interstitial Lung Disease (ILD) are systemic inflammatory conditions that independently increase the risk of Acute Coronary Syndrome (ACS). However, there is a lack of studies examining the risk of mortality and morbidity in patients with both RA and ILD who present with ACS. Hence, our study investigates the increased incidence of ACS in RA patients with ILD, focusing on gender and racial disparities.
Methods: We identified all patients (≥18 years of age) with discharge diagnosis of RA using their respective ICD-9 and ICD-10 codes. Among these patients, we identified patients who had coexisting ILD. Patients with admitting diagnosis of ACS based on the relevant ICD codes were then identified. For baseline characteristics, we used patient demographics (age, race, sex), relevant co-morbidities: peripheral vascular disease, stroke, liver disease, malignancy, hypertension, diabetes mellitus, chronic obstructive pulmonary disease, congestive heart failure, ESRD, hyperlipidemia and obesity. We further grouped patients based on the presence and absence of ILD and analyzed patients for risk of development of ACS and outcomes including all-cause mortality analysis and requirement of percutaneous coronary intervention (PCI) and coronary artery bypass grafting (CABG).
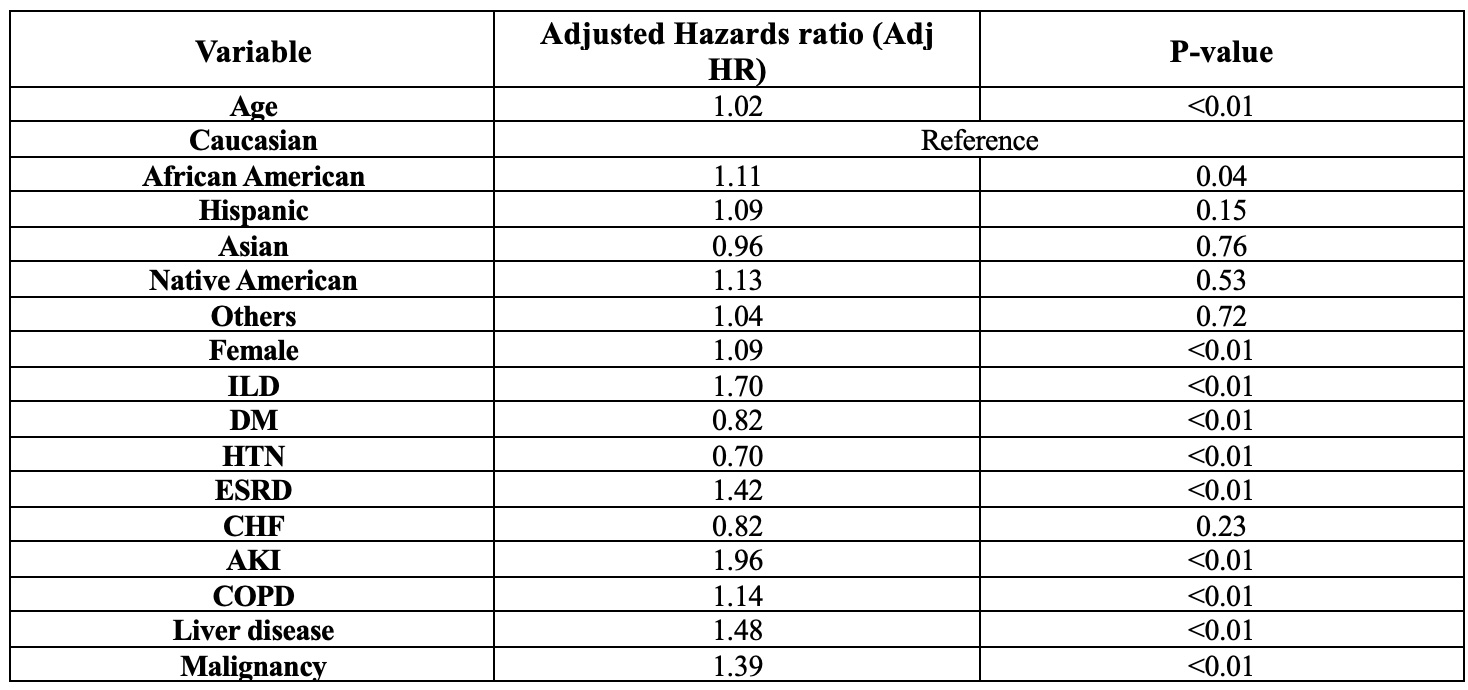
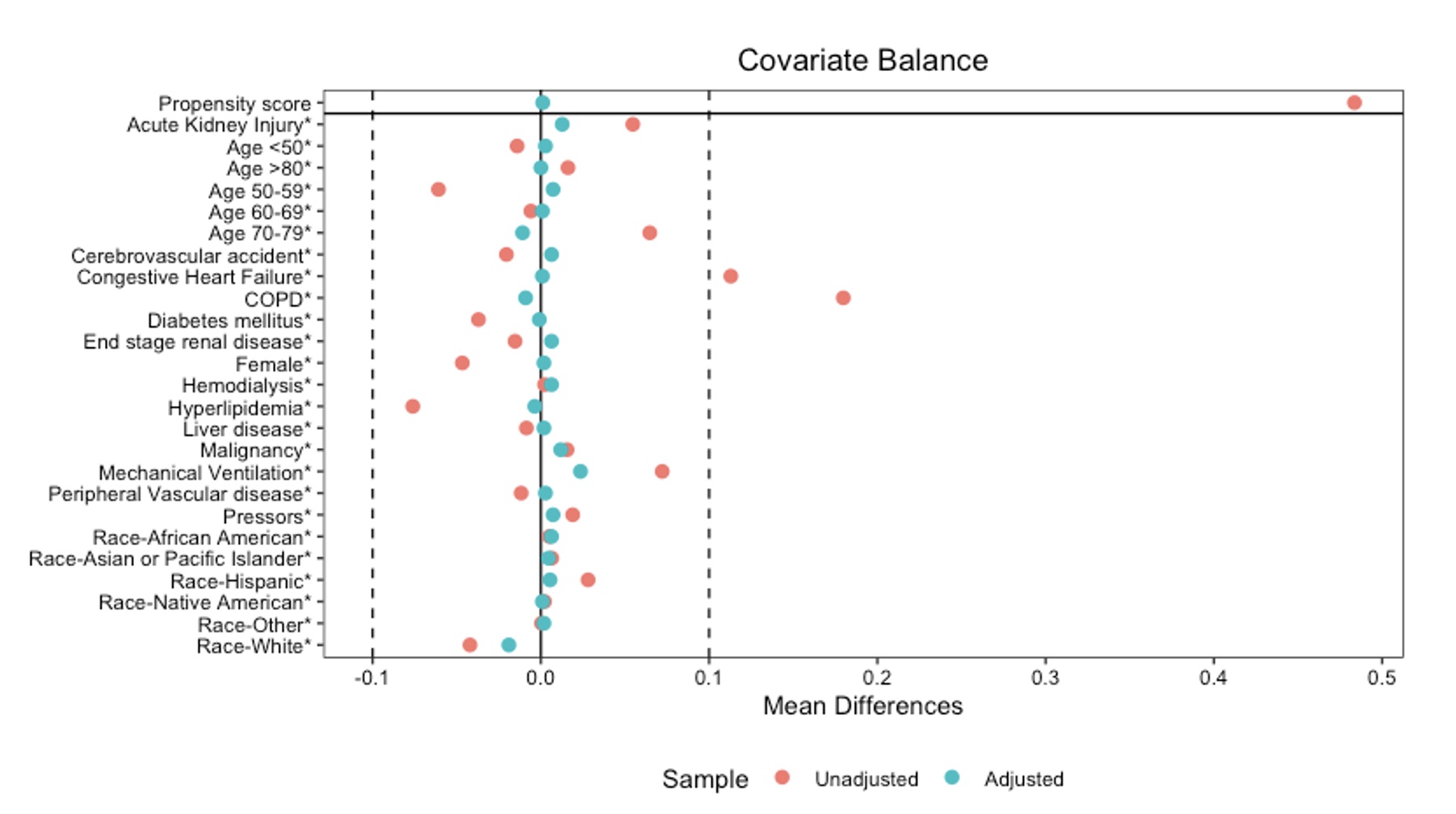
Results: A total of 864,724 patients with RA were identified using ICD codes. Of these, 25064 patients had ILD. Females constituted a higher proportion (N= 642,811; 76.3%). Caucasians were predominant (N= 620,894; 72%) followed by African Americans (n= 105,636; 12.2%). Multivariate regression analysis, adjusting for baseline demographics and traditional risk factors, showed that RA patients with ILD were at increased risk for the development of ACS (adj. HR 1.007; p< 0.01). Furthermore, the presence of ILD was associated with an increased risk of mortality (adj. OR 1.7; p< 0.01) when compared to RA patients with ACS without ILD (Table 1). African American and females were found to be at a higher risk for mortality after adjusting for presence of ILD in RA patients with ACS (Table 1). Propensity score matching analysis matched for 17 different variables including severity confirmed the increased mortality risk (Figure 1). Non-ILD patients with RA and ACS undergo CABG and PCI more than patients with ILD and the patients with ILD had a longer length of stay than the patients without lung disease.
Conclusion: Our study reveals that RA patients with ILD face an elevated risk of developing ACS and a significantly higher risk of mortality and morbidity with increased length of stay. Additionally, our study highlights the need for further research into the gender and racial disparities in this patient group to develop more tailored and effective interventions.
(ILD, Interstitial lung disease; DM, Diabetes mellitus; HTN, Hypertension; CHF, congestive heart failure; ESRD, end stage renal disease; AKI, acute kidney injury; COPD, Chronic obstructive pulmonary disease)
To cite this abstract in AMA style:
Khan O, Naeem A, Jana K, Baqir S, Shyam T, Nanda S. A Nationwide Analysis of Risk of Acute Coronary Syndrome in RA Patients with Interstitial Lung Disease [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/a-nationwide-analysis-of-risk-of-acute-coronary-syndrome-in-ra-patients-with-interstitial-lung-disease/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/a-nationwide-analysis-of-risk-of-acute-coronary-syndrome-in-ra-patients-with-interstitial-lung-disease/