Session Information
Session Type: Poster Session (Sunday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Anti-ribosomal P (Rib-P) antibodies have become known as a highly specific biomarker for the diagnosis of SLE and potentially a biomarker for neuropsychiatric SLE (NPSLE). However, despite comparable specificity in comparison to other SLE autoantibodies such as anti-Sm and anti-dsDNA, anti-Rib-P has not been included in classification criteria for SLE. One limitation has been the wide variation of immunoassays and antigenic targets used to detect anti-Rib-P. Furthermore, the definition of NPSLE encompasses a broad spectrum of neuropsychiatric symptoms. To clarify the clinical associations in SLE, we performed a systematic review and meta-analysis to compare the different anti-Ribo-P assay platforms, antigenic targets, and specific clinical features of SLE and NPSLE.
Methods: PubMed, EMBASE, and Web of Science databases were searched. Associations with clinical features of SLE with attention to specific neuropsychiatric symptoms, type of immunoassays and antigenic targets were extracted. Data were pooled using random effects methods. Associations were expressed as pooled odds ratio (OR) and forest plots to visualize the results.
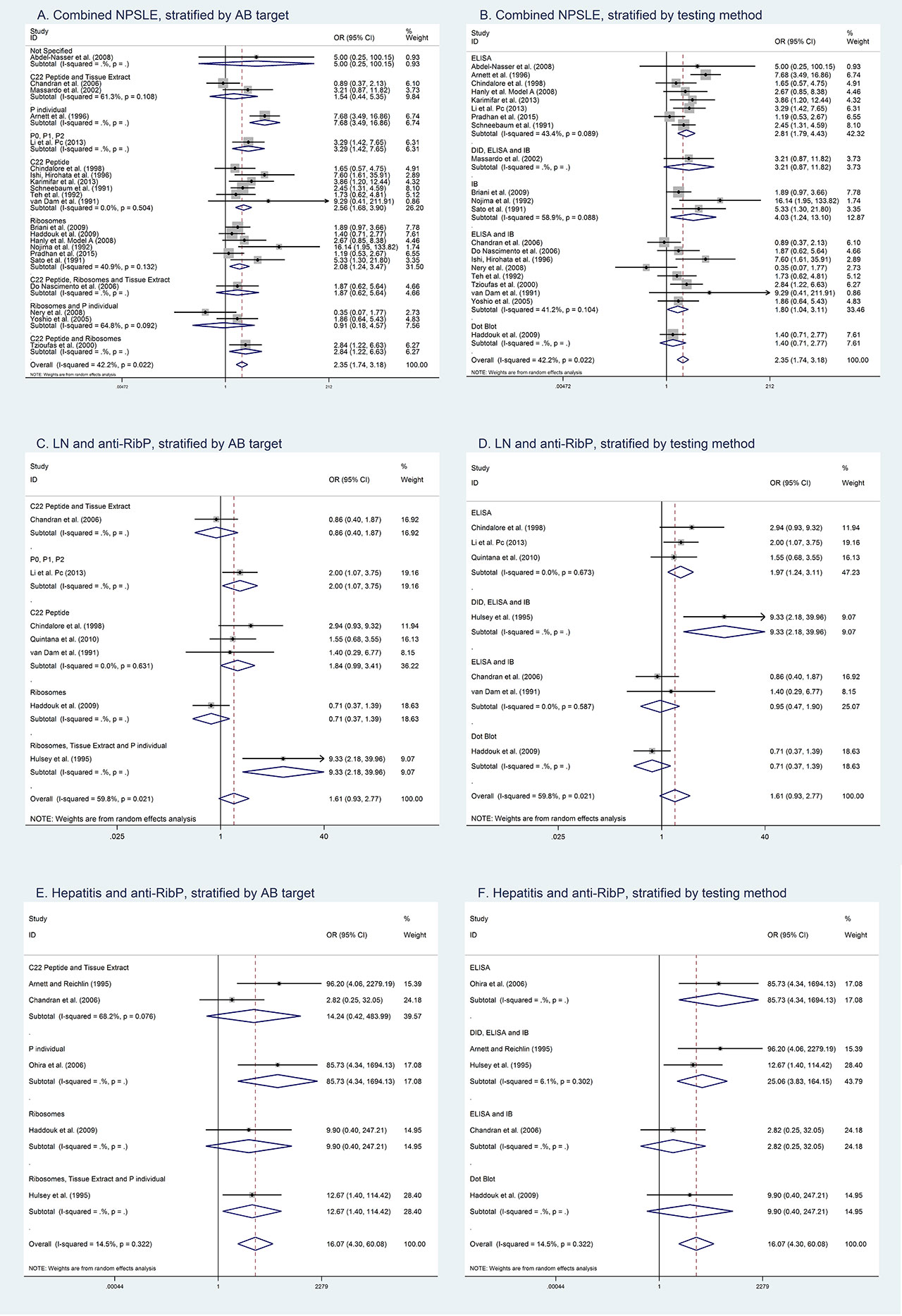
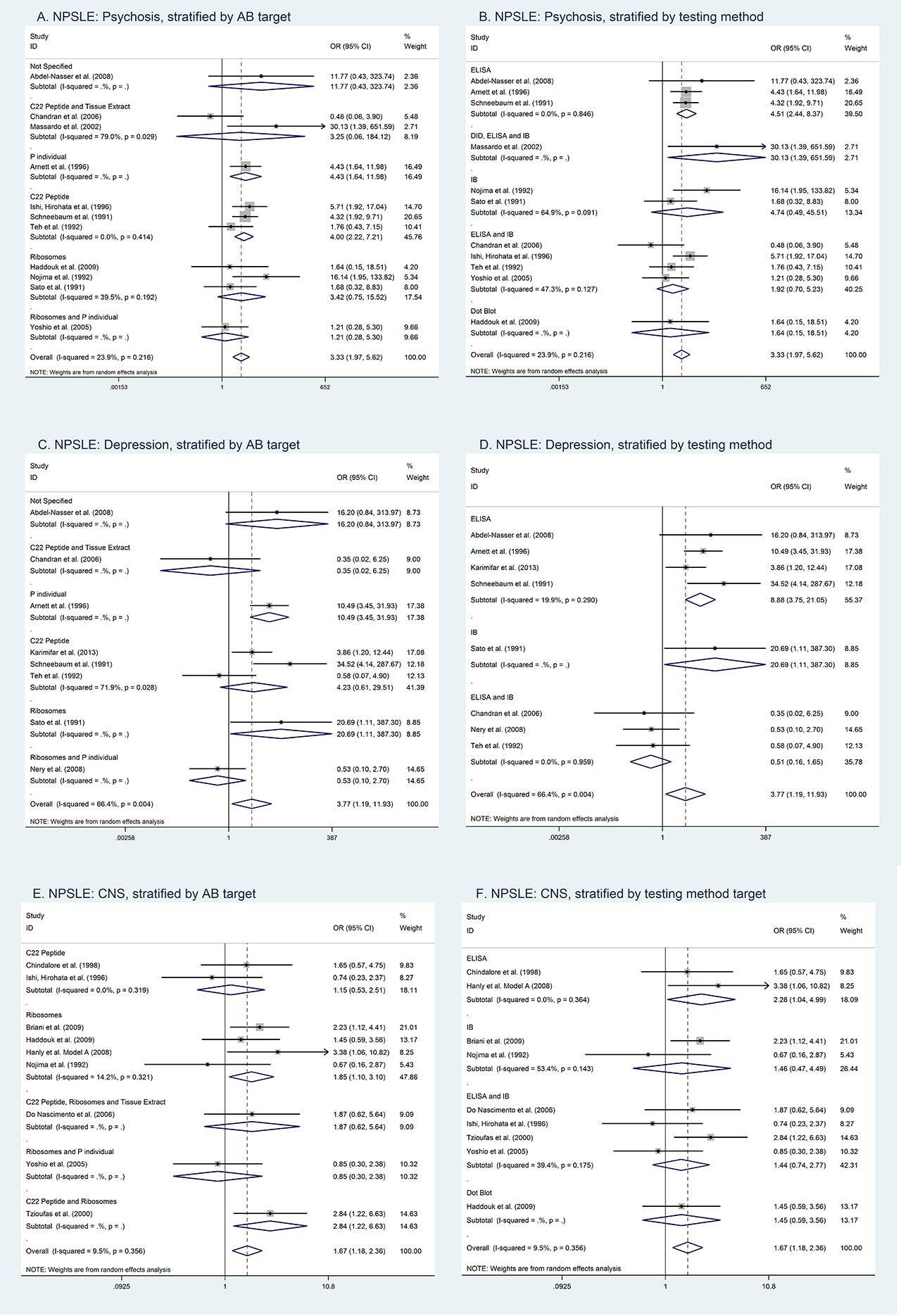
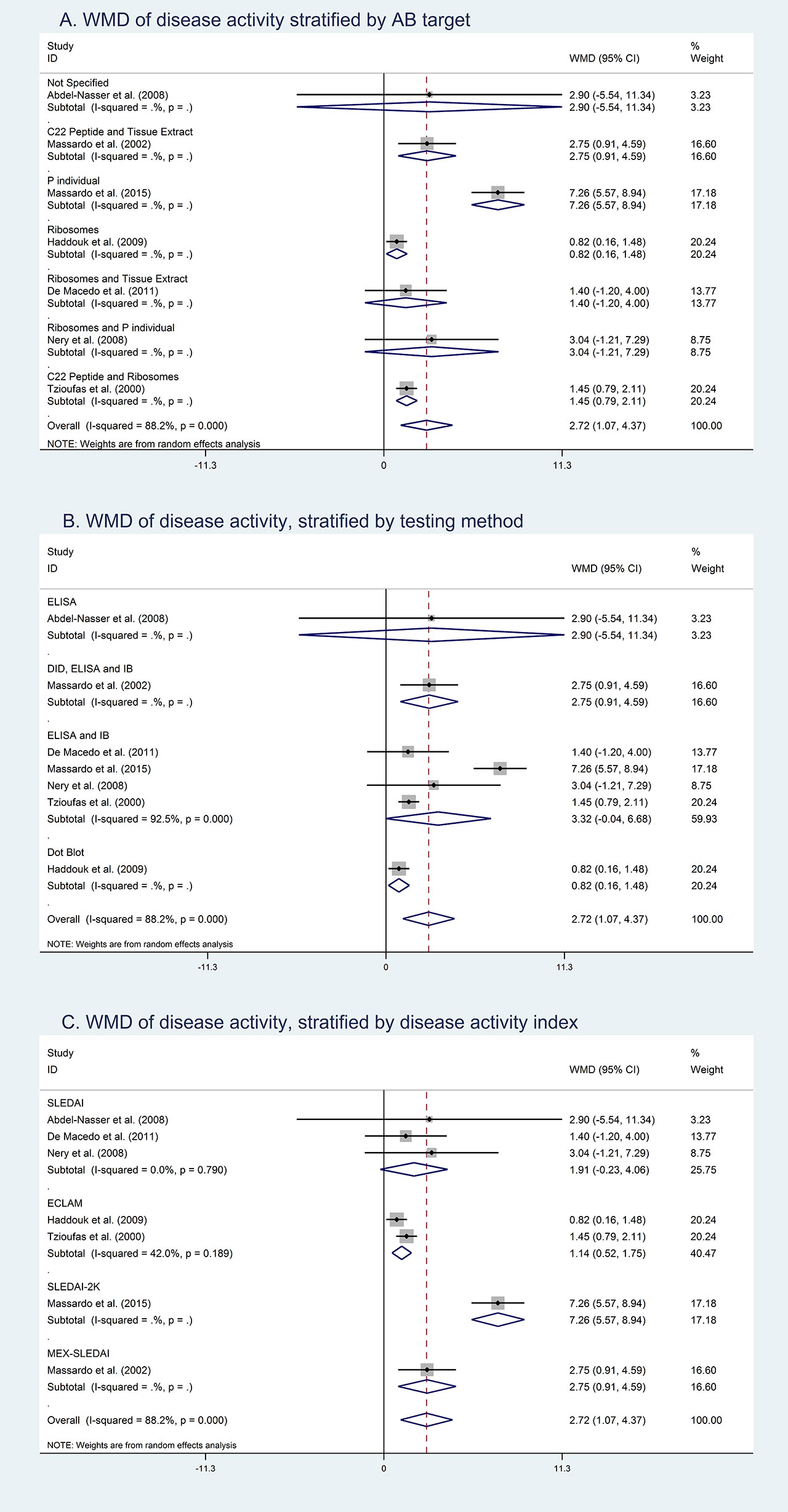
Results: Our preliminary search identified 21 studies (n=3128) that reported a pooled OR of anti-Rib-P positivity in NPSLE of 2.36 (95% confidence interval (CI): 1.74-3.18) (Figure 1). When stratified by different symptoms of NPSLE, depression had the highest pooled OR of 3.77 (95% CI: 1.19-11.93), followed by psychosis (OR 3.33 (95% CI: 1.97-5.62)), and then central nervous system (CNS) involvement (OR 1.65 (95% CI: 1.11-2.45)) (Figure 2). There were 7 studies (n=1060) that reported a pooled OR for lupus nephritis (LN) of 1.61 (95%CI: 0.93-2.77) and 5 small studies (n=504) that reported a pooled OR for lupus hepatitis of 16.07 (95% CI: 4.30-60.08). Seven studies reported that anti-Rib-P was associated with increased disease activity, however, we were not able to pool the results because different disease activity scores were used (SLEDAI, ECLAM, SLEDAI 2K or MEX-SLEDAI) (Figure 3). There was significant heterogeneity between studies that was at least partly explained by heterogeneity in antigenic targets (C22 peptide, ribosomes, P0/P1/P2, tissue extract, and P individual) and assays (double diffusion, enzyme-linked immunosorbent assay, immunoblot, and/or dot blot) used for these studies.
Conclusion: The addition of anti-Rib-P may improve the specificity of SLE classification criteria in patients presenting with NPSLE symptoms. Anti-Rib-P was also found to be an important biomarker for lupus hepatitis and potentially disease activity. Heterogeneity between studies in this meta-analysis is explained by different assays and antigenic targets.
To cite this abstract in AMA style:
Choi M, Brown R, Buhler K, Mahler M, Fritzler M. A Meta-Analysis of Anti-Ribosomal P Autoantibodies in Systemic Lupus Erythematosus: A Misunderstood Autoantibody [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/a-meta-analysis-of-anti-ribosomal-p-autoantibodies-in-systemic-lupus-erythematosus-a-misunderstood-autoantibody/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/a-meta-analysis-of-anti-ribosomal-p-autoantibodies-in-systemic-lupus-erythematosus-a-misunderstood-autoantibody/