Session Information
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: Physical examination of a patient with nonspecific shoulder pain is a non-standardized teaching objective among rheumatology fellowship programs. We used the Delphi methodology to identify both variability in shoulder examination performed by rheumatology fellows and areas of consensus among rheumatology fellowship program directors (PDs) in New England.
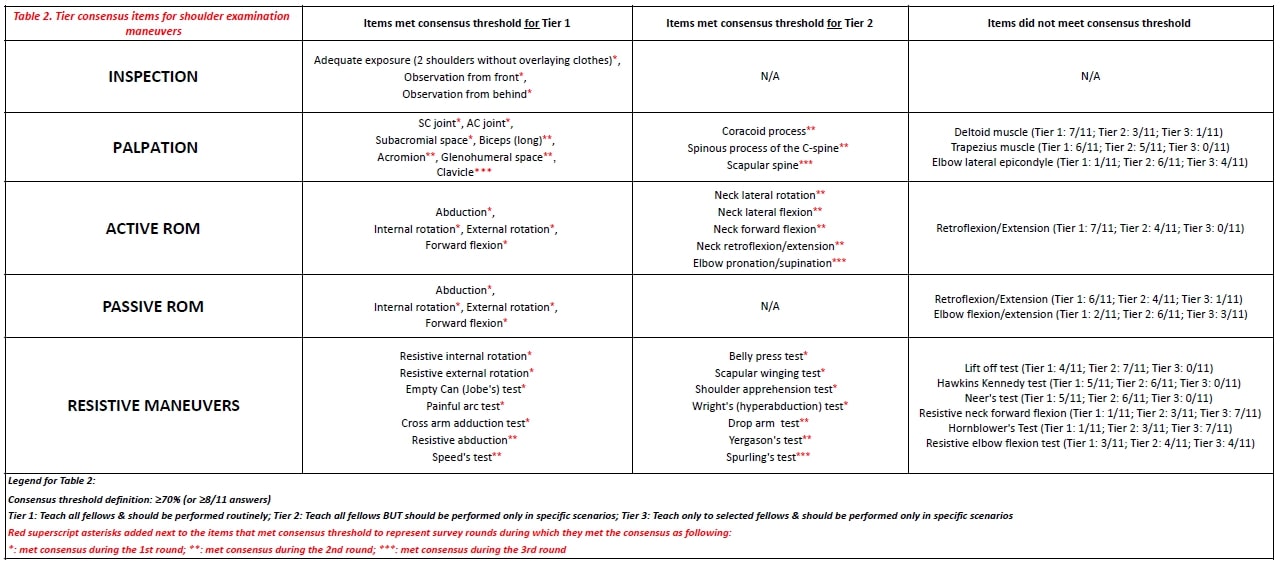
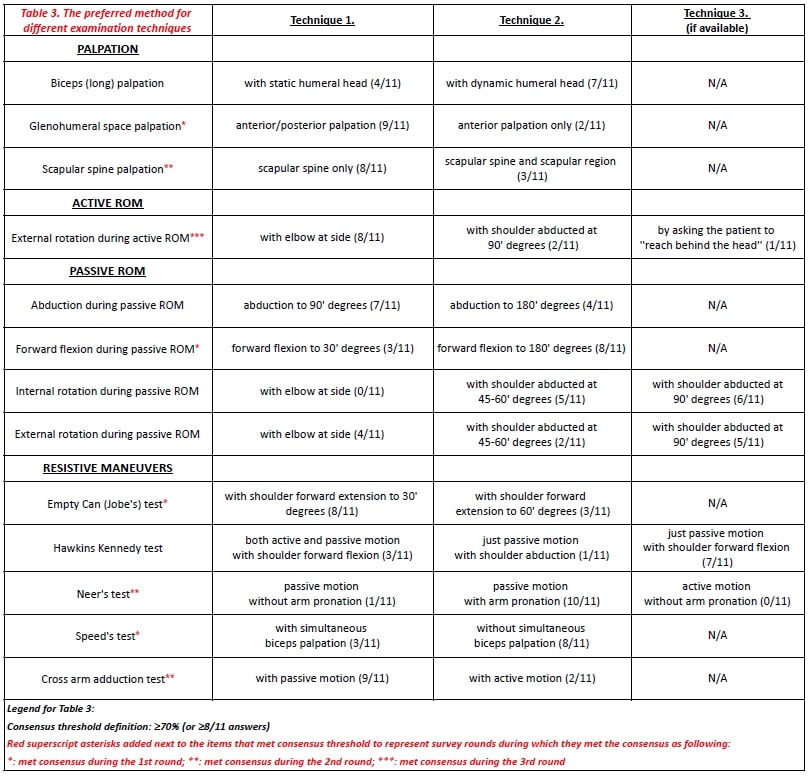
Methods: Past or present rheumatology PDs currently working in New England were recruited. Participants taught a 5-minute shoulder examination to one of their trainees and recorded the resulting video of the shoulder examination by the trainee. We compiled a comprehensive list of all the performed maneuvers from these videos. Participants received an anonymized electronic survey instructing them to rank each maneuver into one of the three categories: (Tier 1) Teach all fellows & should be performed routinely; (Tier 2) Teach all fellows BUT should be performed only in specific scenarios; (Tier 3) Teach only to selected fellows & should be performed only in specific scenarios. When a significant variation in technique between trainees was observed, we surveyed PDs for the best technique (independently of the results of tier consensus). We encouraged participants to include comments explaining reasoning, and/or literature support for their choices. Participants received a compilation of anonymized comments and results of the 1st survey round. Items not meeting ≥70% consensus threshold were included in the 2nd survey. This process was repeated for a 3rd survey. A separate survey collected PD demographics.
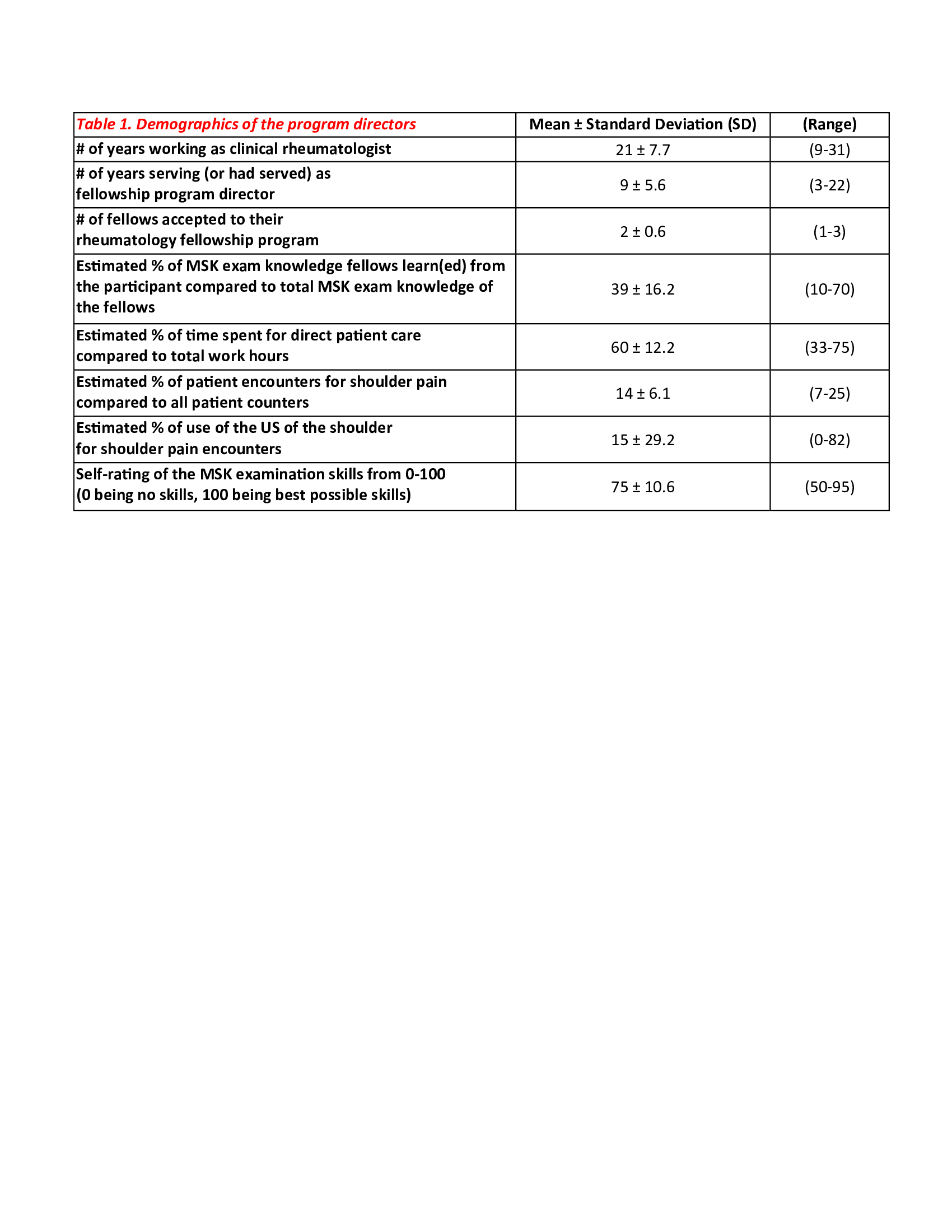
Results: 11 of 13 recruited PDs agreed to participate and 100% of participants completed all rounds of the study. Participants were PDs for nine years (range 3-22), 45% are/were the main teachers for the MSK examination in their fellowship programs, andrated themselves 75 (range 50-95) on a 100-point scale for prowess in physical examination (Table 1). The study addressed 65 items: 52 questions for tier designation of the exam maneuvers and 13 questions for different examination techniques. Participants achieved consensus for 40/52 tier designation items (Table 2) and for 8/13 technique items (Table 3). Consensus for tier designation items increased from 44% in round 1, to 69% in round 2, and 77% by round 3. For technique-related items, consensus increased from 31% to 54% to 61% (Tables 2 and 3).
Conclusion: This is the first study focused on shoulder examination specific to rheumatology training and practice, which may be distinct from that required for orthopedics, physiatry, or primary care. By collecting anonymized video recordings from each participant, we cataloged the range of shoulder physical exam maneuvers and techniques performed in almost all teaching programs in New England. The Delphi methodology allowed consensus building among PDs for which shoulder examination techniques to teach, which to perform routinely vs. selectively, and how to perform them. These results, in the context of ”nonspecific” shoulder pain, should be generalizable and can provide guidance for all US rheumatology fellowship training programs given the similarity in the scope of practice and education.
To cite this abstract in AMA style:
Degirmenci H, Kalish R, Chopra R, Gilek-Seibert K, Koumpouras F, Kyttaris V, Lakshminarayanan S, Libman B, Mathew S, O'Rourke K, Reginato A, Kissin E. A Consensus Based Shoulder Examination for Rheumatology Training [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/a-consensus-based-shoulder-examination-for-rheumatology-training/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/a-consensus-based-shoulder-examination-for-rheumatology-training/