Session Information
Session Type: Abstract Session
Session Time: 2:00PM-3:30PM
Background/Purpose: Over the last decade, lung disease (LD) has become an increasingly recognized complication of systemic juvenile idiopathic arthritis (sJIA). Children with sJIA-LD may be asymptomatic (diagnosed based on chest imaging) or present with a rapidly progressive disease course that can be fatal. Currently, the true burden of disease is unknown due to the variability of clinical symptoms and lack of a standardized approach to pulmonary screening in sJIA patients. Here, we sought to develop an algorithm to evaluate for LD in patients with sJIA at our institution.
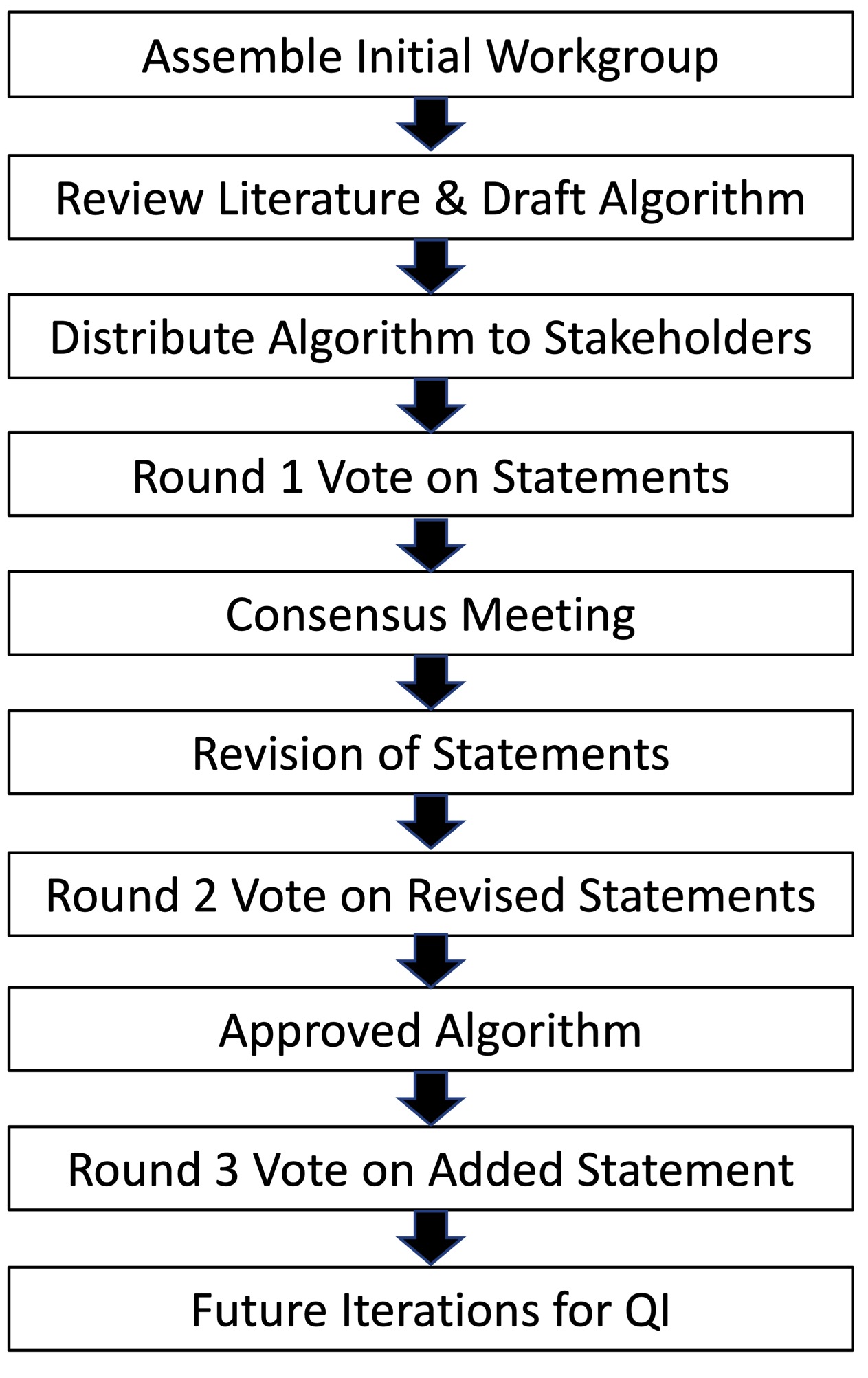
Methods: A multidisciplinary workgroup was assembled and included members representing rheumatology (n=14), pulmonary (n=5), stem cell transplantation (n=1), and patients and their families (n=2). Four workgroup leaders drafted an initial algorithm based on review of the published literature and experience at our center. A modified Delphi approach was used to achieve agreement through 3 rounds of anonymous, asynchronous voting and a consensus meeting held in the Fall of 2022 (Figure 1). Approved statements were rated as appropriate by the workgroup with moderate or high levels of consensus. These approved statements were organized into the final version of the screening algorithm for LD in sJIA.
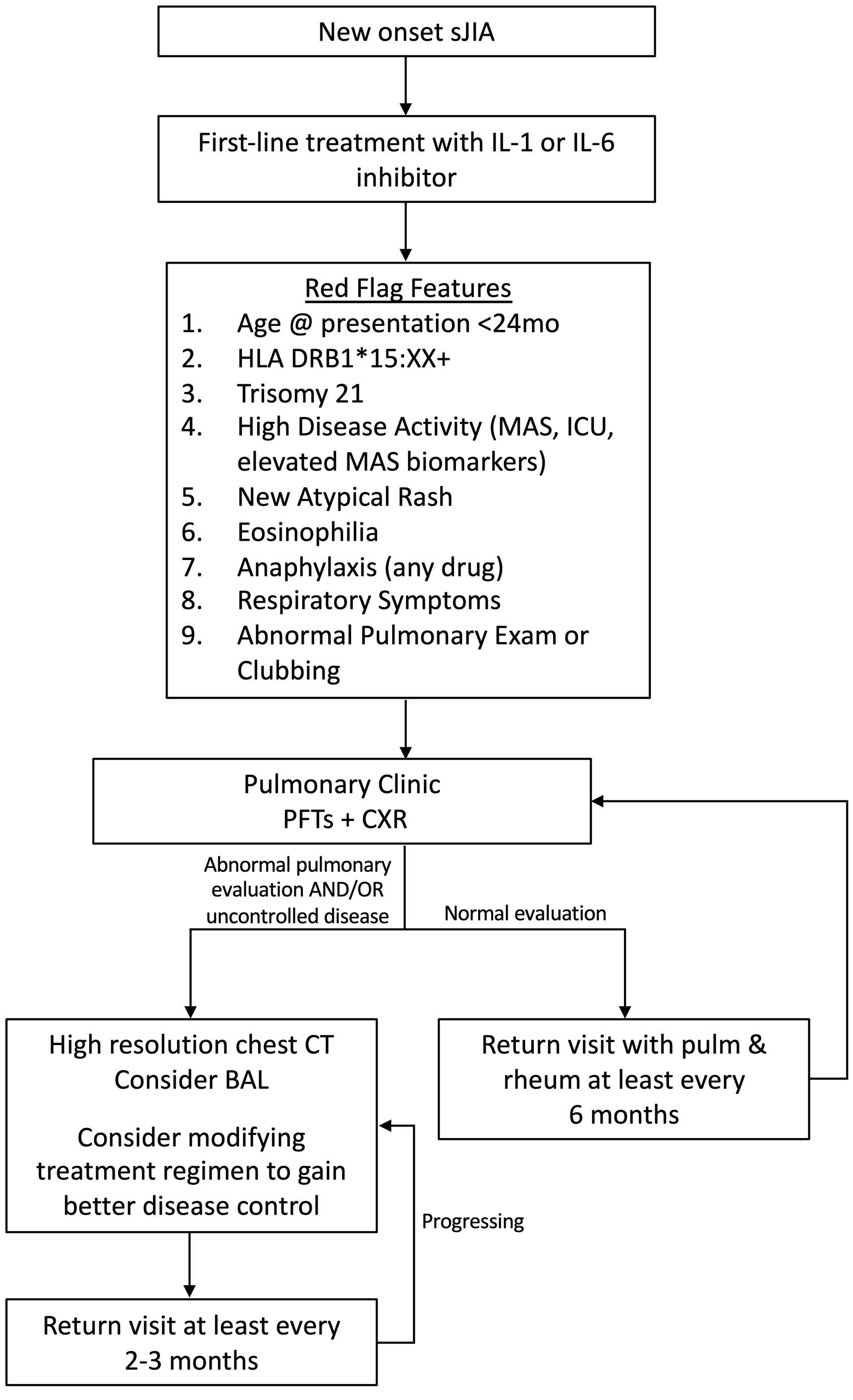
Results: The workgroup ultimately rated 21 statements as appropriate with a moderate or high level of consensus. The final algorithm recommends pulmonary screening for newly diagnosed sJIA patients with clinical features that the workgroup agreed may confer increased risk for LD (Figure 2). These “red flag” features include: baseline characteristics (young age at sJIA disease onset, presence of HLA-DRB1*15 alleles, trisomy 21), high disease activity (history of MAS, sJIA-related ICU admission, elevated MAS biomarkers such as ferritin, soluble IL-2 receptor, IL-18 and CXCL9), respiratory symptoms or abnormal pulmonary examination findings, and features of drug hypersensitivity-like reactions (eosinophilia, new non-evanescent rash without identifiable cause, anaphylaxis to any drug). The presence of any red flag feature prompts an initial pulmonary evaluation, which includes pulmonary function tests (3-minute walk test for young children who cannot perform PFTs), chest x-ray, and referral to the pulmonary clinic. For patients with an abnormal initial pulmonary evaluation and/or persistently active sJIA disease, a high-resolution chest CT is recommended. Bronchoalveolar lavage should also be considered in these patients to evaluate for infectious causes of respiratory decline. The workgroup recommended that all patients with red flag features should be followed closely in the pulmonary clinic.
Conclusion: We used a multidisciplinary, consensus-based approach to develop a strategy to screen for LD in children with sJIA. This approach is intended to reduce practice variation and identify pulmonary complications earlier in the disease course when interventions may be more successful. The algorithm will form the foundation upon which iterative changes can be made as our understanding of sJIA-LD improves.
sJIA-LD, systemic juvenile idiopathic arthritis lung disease; QI, quality improvement
This algorithm was developed for educational purposes only and for use in the Rheumatology and Pulmonary Programs at Boston Children’s Hospital. Decisions about evaluation and treatment are the responsibility of the treating clinician and should always be tailored to individual clinical circumstances.
sJIA, systemic juvenile idiopathic arthritis; ICU, intensive care unit; MAS, macrophage activation syndrome; AEC, absolute eosinophil count; sIL_2R, soluble IL_2 receptor; PFTs, pulmonary function tests; CXR, chest x-ray, CT, computed tomography; BAL, bronchoalveolar lavage; DLCO, diffusing capacity of the lungs for carbon monoxide
To cite this abstract in AMA style:
Wobma H, Bachrach R, Farrell J, Chang M, Day-Lewis M, Dedeoglu F, Fishman M, Halyabar O, Harris C, Ibanez D, Kim L, Klouda T, Krone K, Lee P, Lo M, McBrearty K, Meidan E, Prockop S, Samad A, Son M, Nigrovic P, Casey A, Chang J, Henderson L. A Consensus Based Algorithm to Screen for Lung Disease in Children with Systemic Juvenile Idiopathic Arthritis [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/a-consensus-based-algorithm-to-screen-for-lung-disease-in-children-with-systemic-juvenile-idiopathic-arthritis/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/a-consensus-based-algorithm-to-screen-for-lung-disease-in-children-with-systemic-juvenile-idiopathic-arthritis/