Session Information
Session Type: Poster Session B
Session Time: 8:30AM-10:30AM
Background/Purpose: In other conditions that require chronic management, poor retention in ambulatory care is associated with adverse outcomes. We previously identified that living in the most disadvantaged neighborhoods was the greatest predictor of poor care retention among lupus patients in one urban cohort. Given high hospitalization and rehospitalization rates among lupus patients, this study aims to measure rates and predictors of retention in lupus care prior to hospitalization. Results will inform efforts to improve care retention, health disparities, and outcomes for patients with lupus.
Methods: This retrospective cohort study used a 20% random Medicare sample of adult hospitalizations with an SLE diagnosis code from 2013-2014. Inclusion required at least one year of continuous Medicare AB coverage before hospitalization.
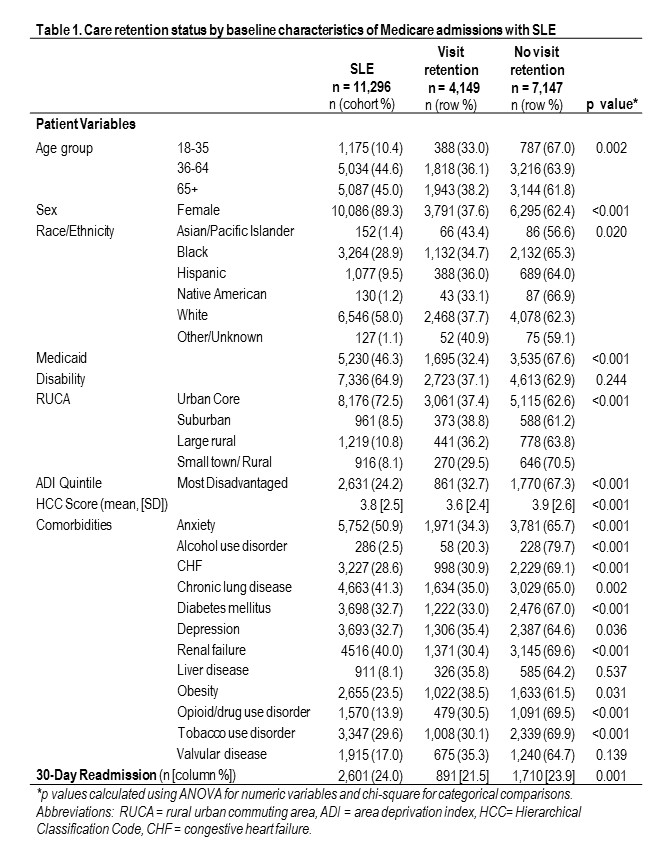
Retention in lupus care was measured in the 12 months prior to hospitalization. Visit-based retention in care used an established threshold of at least two ambulatory rheumatologist visits >= 90 days apart. Rates of visit-defined care retention were calculated by sociodemographic and comorbidity groups. Generalized logistic regression, clustered by patient, was performed to identify predictors of care retention.
Results: Among 11,296 SLE-related hospitalizations, the overall observed rate of visit-defined care retention in the year prior to hospitalization was just 36.7%. White, Black, and Hispanic patients had lower rates of retention when compared to Asian/Pacific Islander patients (37.7%, 34.7%, 36.0% vs. 43.4% p=0.02, Table 1). Retention rates for rural-residing patients were significantly lower than suburban (29.5% vs 38.8%, p < 0.001). Hospitalizations associated with the most disadvantaged neighborhood ADI quintile had lower rates of patient retention (32.7% vs 38.5%, p < 0.001). Thirty-day rehospitalization rates were 21.5% among those with baseline retention compared to 23.9% without.
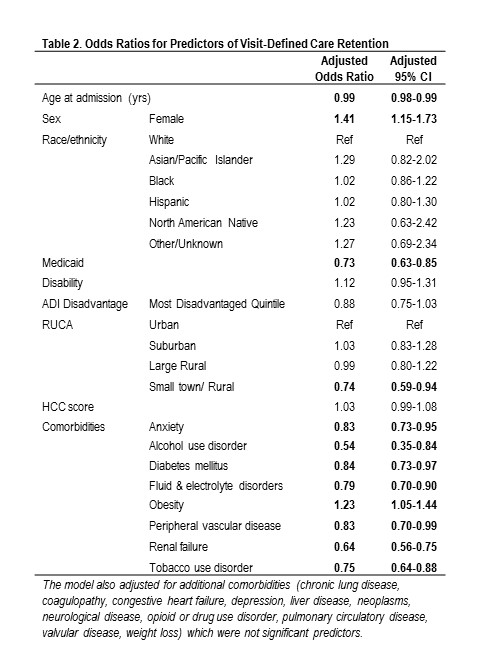
Multivariable analysis showed that women were more often retained (aOR 1.41, 95% CI 1.15-1.73) (Table 2). Rural residents had 26% lower odds of being retained in care when compared to urban residents (0.74, 0.59-0.94). History of Medicaid enrollment, a proxy of low SES, was significantly associated with decreased odds of retention in care (0.73, 0.63-0.85). Similarly, alcohol use (0.54, 0.35-0.84), tobacco use disorders (0.75, 0.64-0.88), and renal failure (0.64, 0.56-0.75) were associated with lower odds of retention in care. Obesity predicted 23% greater odds of retention (1.23, 1.05-1.44). Race/ethnicity and ADI quintile were not significant in the full model. Limitations include potential misclassification of NP/PA visits.
Conclusion: Rural residence and lower SES, indicated by Medicaid eligibility, predicted lower likelihood of retention in ambulatory lupus care prior to hospitalization. Several comorbid conditions, including renal failure, also predicted lower retention. Those retained in care had lower rates of 30-day readmission. Findings highlight the importance of addressing ambulatory access and outreach to retain and re-engage lupus patients in rheumatology care. Results can aid patient-provider communication on the importance of continuity of lupus care.
To cite this abstract in AMA style:
Schletzbaum M, Torres C, Kind A, Gilmore Bykovskyi A, Sheehy A, Bartels C. A Cohort Study of Retention in Ambulatory Lupus Care Among Medicare Patients with SLE-related Hospitalizations [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/a-cohort-study-of-retention-in-ambulatory-lupus-care-among-medicare-patients-with-sle-related-hospitalizations/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/a-cohort-study-of-retention-in-ambulatory-lupus-care-among-medicare-patients-with-sle-related-hospitalizations/