Session Information
Session Type: Abstract Submissions (ACR)
Background/Purpose: Psoriatic arthritis mutilans (PAM) is a rare extreme subtype of psoriatic arthritis (PsA). Our objectives were to: (1) compare clinical characteristics of PsA patients with PAM and without PAM (non-PAM); (2) determine the rate of PAM radiographic progression.
Methods: A retrospective cohort study was conducted of all PsA patients attending a teaching hospital. Clinical characteristics were recorded. Most recent radiographs of hands and feet were evaluated for PAM, defined as osteolysis affecting ≥50% of the articular surface on both sides of the joints. All available radiographs (earliest to most recent) were quantitatively scored for osteolysis, erosion, joint space narrowing, and osteoproliferation. Radiographic progression was analysed using random effects models to allow for patient differences, and additive models for all joints.
Results: 610 PsA cases fulfilling CASPAR criteria were screened: 36 PAM (35 with serial radiographs); 483 non-PAM; 91 had insufficient radiographs to determine PAM.
PAM cases were younger at diagnosis of PsA than non-PAM cases (33 vs. 40 years; p=0.04). Psoriatic nail dystrophy was more prevalent in PAM than non-PAM cases (83.33 vs. 47.95%; p=0.0002). At most recent assessment, PAM cases had a higher HAQ than non-PAM cases (median 1.25 vs. 0.63; p=0.05), especially in domains relating to hand / feet function: HAQ-grip (p=0.02); HAQ-eating (p=0.03). In cases with ACPA serology available, PAM cases were no more likely to be ACPA positive (0/16) than non-PAM cases (8/226; p=0.44). 16/28 PAM cases had radiographic sacroiliitis, often bilateral (14/16) and of grade ≥3 (15/16). During their disease course, PAM cases were more likely than non-PAM cases to have used a DMARD (91.67 vs. 50.21%; p<0.0001), but no more likely to have used a Biological (p=0.53). 87.50% of PAM cases had used a DMARD before PAM-occurrence.
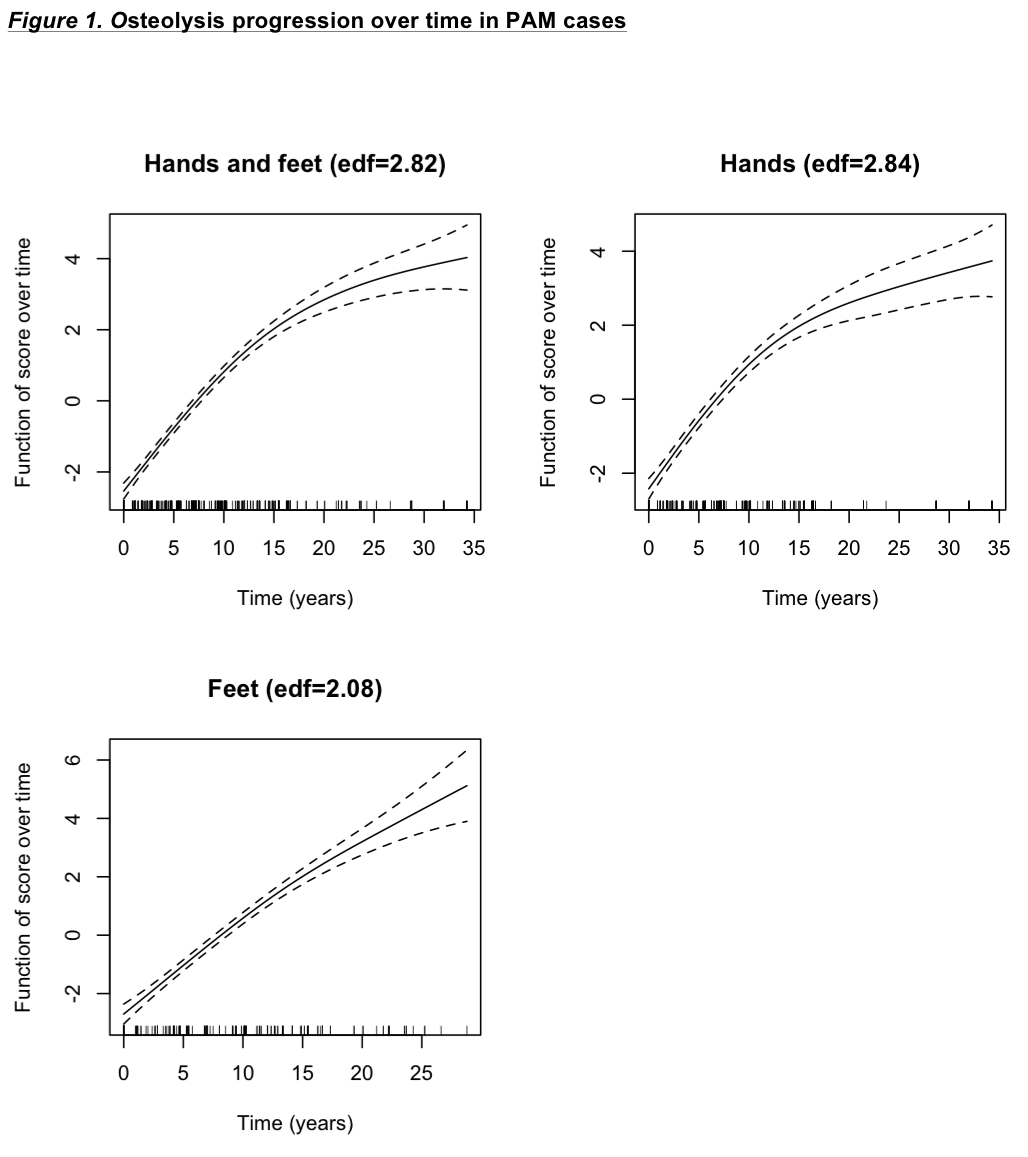
A median of 5 radiographs were scored for each PAM case (IQR 3-7). 22/35 patients developed PAM during the course of their follow-up. PAM was most commonly monoarticular (21/35) at first observation, and polyarticular most recently (28/35). The most frequently affected joints were: feet IPJ1, MTPJ2-5; hand DIPJ2, PIPJ5, MCPJ1. Significant changes in osteolysis scores over time were observed for all joints (p<0.008). There was strong indication of differences in the patterns of deterioration over time for different joints (p<0.001). An initial increase in score, followed by a slower rate of deterioration was seen (effective degrees of freedom; edf 2.82), with the change in rate more marked for hands (edf 2.84) than feet (edf 2.08) (Figure 1).
Conclusion: PAM is associated with worse physical function, more prevalent nail dystrophy, high-grade bilateral sacroiliitis, greater DMARD use and earlier diagnosis when compared to cases without PAM. Osteolysis progresses most rapidly in early disease, slowing in established disease.
Disclosure:
D. R. Jadon,
None;
G. Shaddick,
None;
W. Tillett,
None;
G. Robinson,
None;
C. Cavill,
None;
N. Waldron,
None;
E. Korendowych,
None;
N. J. McHugh,
None.
« Back to 2014 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/psoriatic-arthritis-mutilans-characteristics-and-radiographic-progression/