Session Information
Session Type: Abstract Submissions (ACR)
Background/Purpose: Numerous studies support obesity as a strong risk factor for development and progression of knee osteoarthritis (OA). The potential benefits of massive weight loss, as seen after bariatric surgery, have not been well studied. The study objective is to examine if massive weight loss after bariatric surgery is associated with improved OA symptoms and quality of life (QoL) compared with medical management alone in obese patients.
Methods: A total of 150 patients were screened for clinical and radiographic evidence of OA within the STAMPEDE trial (March 2007 – Jan 2011). The STAMPEDE trial examined the effects of bariatric surgery vs. medical management alone in obese patients with diabetes. 100 patients received bariatric surgery (50 sleeve gastrectomy and 50 Roux-en-Y gastric bypass) and 50 patients were medically managed. Clinical data, medication usage, and QoL scores were collected before and 12 months after intervention. OA was defined by physician diagnosis at an office visit and/or radiographic evidence of OA (joint space narrowing and osteophytes) of the hip, knee, ankle, or foot. The change in 12 month post-intervention SF-36 scores between the surgical group and medically managed group were compared. Scores were compared using linear regression models, adjusting for baseline score. Baseline scores were centered at their median value.
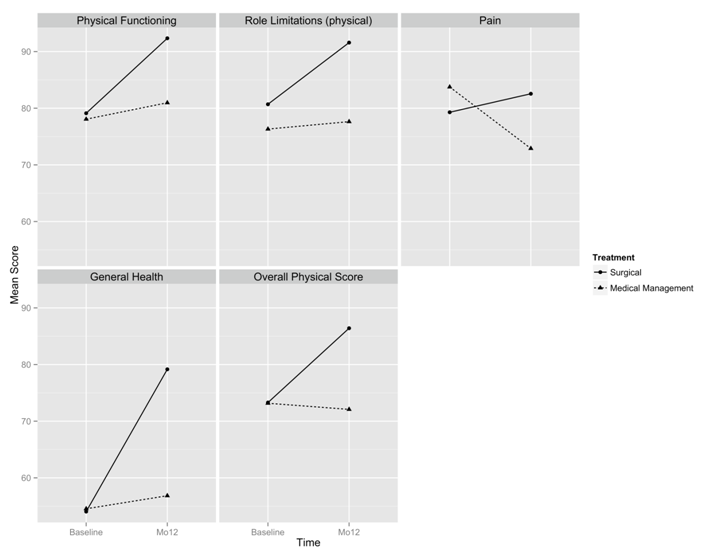
Results: 67 patients with OA had baseline and follow up data available for review. Demographics between the bariatric surgery and medical group were similar (mean age 51, female gender 44/67, mean BMI 36.6). 49 patients were in the surgery group and 18 in the medical group. There was a statistically significant difference in BMI change, over 12 months, between the surgical group and medical group (BMI -9.12 and -2.24 respectively). The surgical group improved in each of the SF-36 physical health scales (Figure 1). There was a significant improvement in the surgical group compared to the medical group in the physical functioning (P 0.03), general health (P <0.001), and overall physical health scores (P 0.004) (Table 1). There was no significant difference between the groups in pain or role-physical scores.
Conclusion: Patients with OA who underwent massive weight loss after bariatric surgery had significant improvement in SF 36 physical functioning and general health scores when compared to patients treated with medical management of weight loss alone. There was also a trend suggesting improvement in bodily pain and role-physical.
|
Table 1: Adjusted SF-36 improvement in surgical compared to medical group at 12 months
|
|||
|
SF-36 Scale |
SF-36 difference |
95% CI |
p-value |
|
Physical Functioning |
11.47 |
1.15 – 21.79 |
0.03 |
|
Role Physical |
8.55 |
-7.12 – 24.21 |
0.28 |
|
Bodily Pain |
9.44 |
-2.77 – 21.65 |
0.13 |
|
General Health |
19.24 |
12.25 – 26.23 |
< 0.001 |
|
Physical Health Summary |
11.87 |
3.94 – 19.81 |
0.004 |
Figure 1: Average SF-36 scores at baseline and 12 months
Disclosure:
C. Chong,
None;
S. Kashyap,
None;
P. Schauer,
None;
C. O’Rourke,
None;
M. E. Husni,
None.
« Back to 2014 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/bariatric-surgery-improves-quality-of-life-in-patients-with-osteoarthritis-and-obesity-compared-to-non-surgical-weight-loss/