Session Information
Session Type: Abstract Submissions (ACR)
Background/Purpose: Several reports show that the presence of comorbidities negatively influences both functional status (1) and quality of life (2) in rheumatoid arthritis (RA). No published study, however, has addressed the impact of comorbidities on the response to biologic treatments. Aim of the present study was to assess whether the presence of arterial hypertension influences the clinical response to biologics in RA.
Methods: The study population consisted of 526 patients affected by RA (416 F 110 M, mean age 53.8±14.27 yrs) treated with first-line biologic treatments. 349 (66.3%) patients were normotensive (NT), and 177 (33.7%) hypertensive (AH). Disease activity was evaluated by DAS28. The 6-month response to biologic treatments was evaluated by EULAR response criteria, and by the percentage of patients in low disease activity (DAS28 <3.2) and in remission (DAS28<2.6). The differences in the percentage of responders between the 2 groups were analyzed by generalized linear models, correcting data for confounder variables (age, sex, baseline disease activity, disease duration), and for the presence of other comorbidities (diabetes, dyslipidemia, ischemic heart disease, osteoporosis, fibromyalgia, thyroid disease and COPD). In the following test, the observed percentages are reported, while statistical significance (p values) refers to corrected values. All statistical analyses were performed with the IBM SPSS 20.0 software.
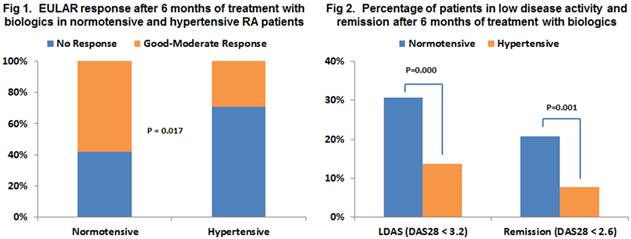
Results: The vast majority of patients were treated with anti-TNF biologics in both groups (AH 94.5%, NT 90.6%, p=0.177). The percentage of females (AH 82% NT F 78%, p=0.586) was not significantly different in the 2 groups, while mean age was significantly higher in AH patients (59.85±12.53 vs 51.29±14.29 yrs, p=0.000), and disease duration in NT patients (4.4±6.4 vs 2.5±5.1 yrs, p=0.001). Among the other comorbidities, only the prevalence of dyslipidemia, osteoporosis, and COPD was significantly higher in AH group (p<0.05). Biologic treatment was stopped or switched in 192/526 (36.5%) patients before the 6th month, without a significant difference between the 2 groups (AH: 75/177 (42.4%); NT 117/349 (33.5%), p=0.361). Baseline DAS28 was higher in AH patients (5.73±1.11 vs 5.18±1.34, p=0.000). EULAR response at 6 months (Fig. 1), and the percentage of patients in low disease activity (14/102 (13.7)% vs 71/232 (30.6%), p=0.000) and in remission (8/102 (7.8%) vs 48/232 (20.7%), p=0.001) (Fig. 2) were significantly lower in AH patients.
Conclusion: Concomitant arterial hypertension influences negatively the response to biologic treatments in rheumatoid arthritis. The presence of comorbidities should be taken into account in the evaluation of the clinical response to biologic treatments.
References:
1) van den Hoek J, et al. Arthritis Care Res (Hoboken). 2013 Jan 17. [Epub ahead of print]
2) Radner H, et al. Rheumatology 2011;50:381–388.
Disclosure:
M. Antivalle,
None;
M. Chevallard,
None;
M. Battellino,
None;
A. Batticciotto,
None;
M. C. Ditto,
None;
A. Mutti,
None;
F. Rigamonti,
None;
V. Varisco,
None;
S. Bongiovanni,
None;
F. Atzeni,
None;
P. Sarzi-Puttini,
None.
« Back to 2013 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/reduced-response-to-biologic-treatments-in-rheumatoid-arthritis-patients-affected-by-arterial-hypertension/