Session Information
Session Type: Abstract Session
Session Time: 12:45PM-1:00PM
Background/Purpose: AxSpA primarily affects the sacroiliac joints and spine, reducing trunk strength, mobility, and cardiorespiratory fitness. While exercise is a key treatment, few studies have examined combined trunk mobility and strength training with cardiorespiratory training. This prospective interventional study assessed the benefits of a combined and personalized exercise intervention based on baseline physical tests.
Methods: Participants with AxSpA completed a baseline maximal Cardiopulmonary Exercise Test (CPET) and trunk strength/mobility tests using David Back Concept (DBC) devices. Strength and mobility deficits were calculated as: (Reference − Patient value) × 100 / Reference. BASDAI, BASFI, BASMI, and chest expansion (CE) were registered pre- and post-intervention. The 8-week program consists of two weekly sessions of two 10-minute intervals of cardiorespiratory training at a set heart rate (HR), followed by DBC device exercises. Cardiorespiratory intensity was based on ventilatory threshold 1 (VT1) and monitored via a Polar HR device. Trunk training focused on mobility and resistance using each patient’s one-repetition-maximum and maximal range of motion at baseline. All sessions were supervised to ensure correct execution and safety. Post-intervention, CPET and DBC tests were repeated. Linear mixed models analyzed changes over time.
Results: Thirty axSpA patients (14M/16F, age 42±11.2 years; BASDAI 3.5±2.1, BASFI 2.8±2.2, BASMI 2.0±1.1, CE 4.5±2.0 cm) participated; 2 patients were lost to follow-up (1: flare, 2: personal reasons). Strength increased on average by 14.1% (p< 0.001), and mobility improved by 14.9% (p< 0.001) on average, with significant time and direction effects.(See Fig.1) Cardiorespiratory parameters improved significantly: oxygen pulse (p=0.004), ventilatory efficiency (p< 0.001), anaerobic threshold (p=0.002), and mechanical efficiency (p=0.021), but not efficiency slope (p=0.888). (See Table 1) BASDAI (2.9±2.2, p=0.021) and CE (5.0±2.1 cm, p=0.020) showed significant improvement, while BASMI (1.8±1.0, p=0.053) showed a borderline significant decrease and BASFI (2.4±2.1, p=0.092) did not differ significantly. (See Table 2)
Conclusion: A combined, individually tailored exercise program, dependent on baseline objectively measured physical parameters, significantly improved cardiorespiratory fitness, trunk strength, and mobility in AxSpA patients. These results support the role of individualized exercise interventions in enhancing patient outcomes and reducing functional limitations.
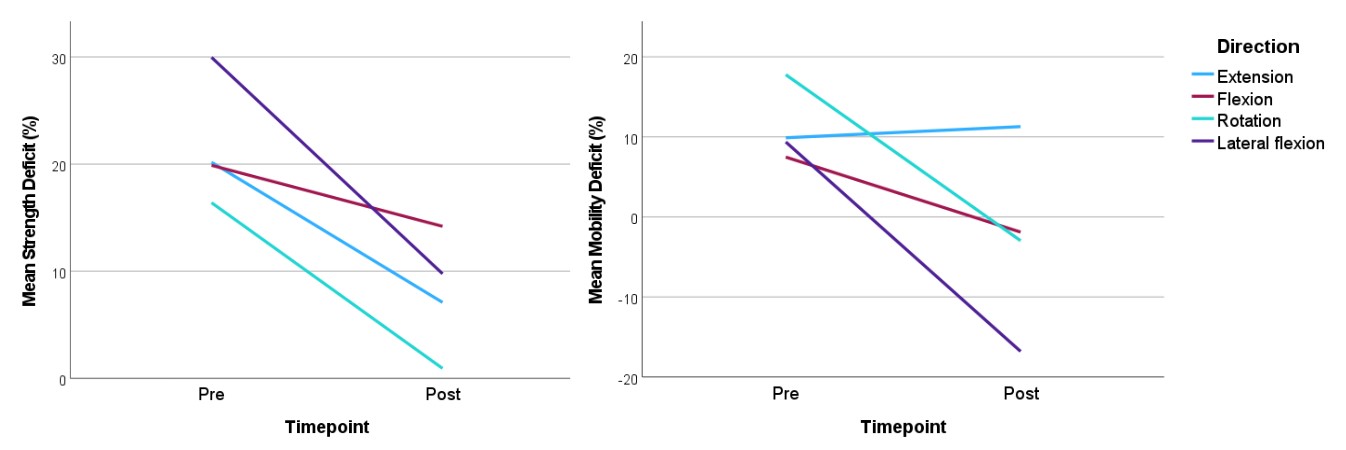 Fig.1: Mean strength (A) and mobility (B) deficit before and after the training program for the different directions.
Fig.1: Mean strength (A) and mobility (B) deficit before and after the training program for the different directions.
.jpg) Table 1: cardiorespiratory parameters before and after intervention
Table 1: cardiorespiratory parameters before and after intervention
.jpg) Table 2: clinical parameters before and after intervention
Table 2: clinical parameters before and after intervention
To cite this abstract in AMA style:
De Mits S, Willems T, Danneels L, Calders P, Varkas G, Van den Bosch F, Elewaut D, Carron P. Individualized Strength, Mobility and Aerobic Rehabilitation Training in axial Spondyloarthritis (iSMART in axSpA) [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/individualized-strength-mobility-and-aerobic-rehabilitation-training-in-axial-spondyloarthritis-ismart-in-axspa/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/individualized-strength-mobility-and-aerobic-rehabilitation-training-in-axial-spondyloarthritis-ismart-in-axspa/
