Session Information
Date: Tuesday, October 28, 2025
Title: (2377–2436) Systemic Lupus Erythematosus – Diagnosis, Manifestations, & Outcomes Poster III
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Systemic lupus erythematosus (SLE is an autoimmune disease that attacks different organs. There have been reports of hyperglycemic hyperosmolar syndrome (HHS) from steroid use in SLE and insulin resistance in SLE, which results in DKA. However, the exact incidence and outcomes of DKA/HHS are unknown.
Methods: This population-based retrospective cohort study utilizes data from the National Inpatient Sample (NIS) database for the period 2021-2022. Patients hospitalized with DKA and HHS based on ICD-10 were identified. Patients were stratified into groups with and without SLE. The primary outcome is the incidence of patients with DKA/HHS and SLE. Secondary outcomes include mortality rate, length of stay (LOS), cost of hospitalization and risk of developing sepsis/septic shock, acute kidney injury, myocardial infarction, acute hypoxic respiratory failure (AHRF), deep vein thrombosis, pulmonary embolism, congestive heart failure, and peripheral vascular disease. Confounders were adjusted using multivariable logistic analysis.
Results: The study included 315435 DKA patients, 95290 HHS patients, and 246427 SLE patients. The incidence of DKA and HHS in SLE is 0.3% and less than 0.01%, respectively. Table 1 summarizes the characteristics of the patients, Table 2 and Table 3 summarize primary and secondary outcomes of interest.DKA patients with SLE were predominantly women (86.43% vs 49.32%, p< 0.01) with younger age (52.93=-1.02 vs 57.20 vs 1.02; p< 0.01) with no difference in racial distribution compared to non-SLE. They were more likely to have diabetes with complications (48.57% vs 37.10%. p=0.049) and long-term steroid use (8.57% vs 0.74%, p< 0.01), but less likely to have renal disease (17.4% vs 35.00%, p< 0.01%) as co-morbidities compared to those without SLE. No difference in the average LOS and the cost of hospitalization was observed. DKA patients with SLE had a significantly higher risk of developing AHRF (aOR=1.67, 95% CI 1.01-2.76, p=0.045). No significant increased risk of mortality (aOR=1.7, 95% CI 0.86-3.36, p=0.13) and risk of other in-hospital outcomes were detected.HHS patients with SLE demonstrated no significant difference in gender, age, and racial distribution. They were more likely to have essential hypertension (50.0% vs 23.16%, p=0.04), insulin use (50.0% vs 21.41%, p=0.02), and long-term steroid use (5.88% vs 0.78%, p< 0.01) as co-morbidities compared to those without SLE. No difference in the average LOS and the cost of hospitalization was observed. HHS patients with SLE had a significantly lower risk of developing AKI (aOR=0.25, 95% CI 0.10-0.64, p< 0.01). No significantly increased risk of other in-hospital outcomes was detected.
Conclusion: DKA patients with SLE had a higher risk of developing AHRF, while HHS patients with SLE have a higher risk of AKI without significant difference in mortality, LOS and cost.
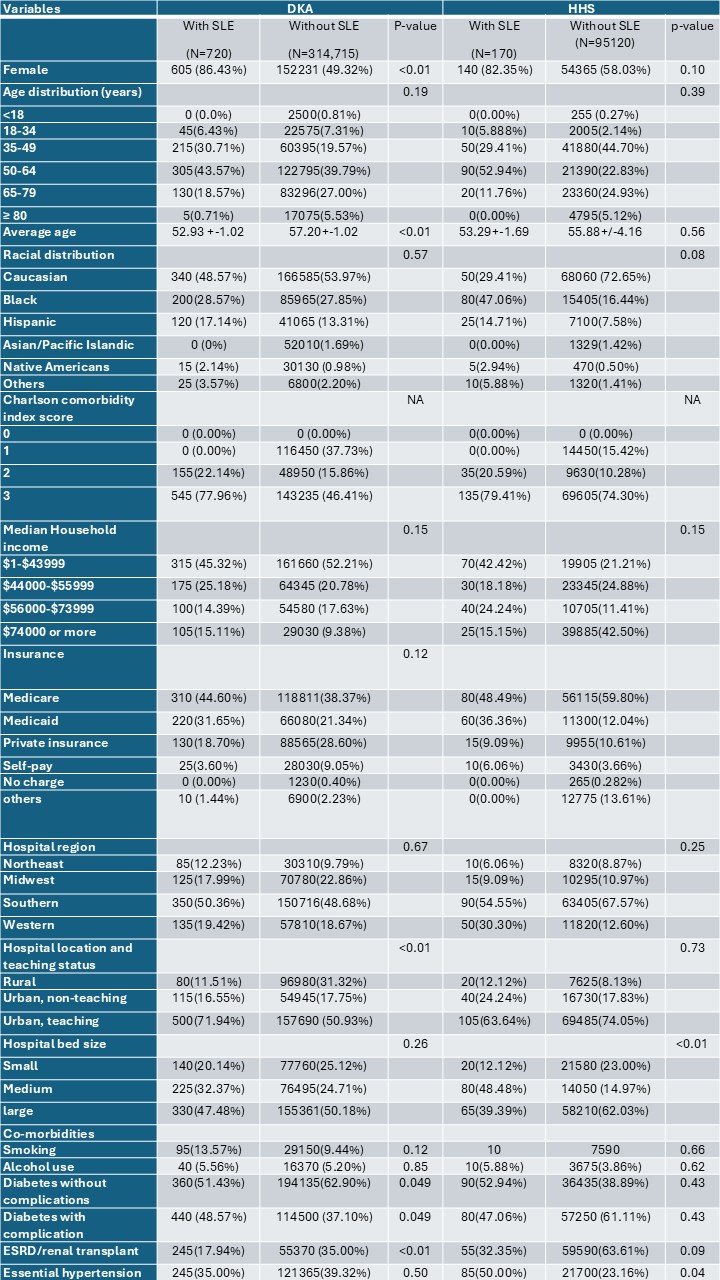 Table 1: Baseline characteristics of patients hospitalized with DKA and HHS with versus without SLE
Table 1: Baseline characteristics of patients hospitalized with DKA and HHS with versus without SLE
.jpg) Table 2: Primary and secondary in-hospital outcomes for DKA and HHS with SLE versus without SLE
Table 2: Primary and secondary in-hospital outcomes for DKA and HHS with SLE versus without SLE
.jpg) Table 3: Outcomes of in-hospital DKA/HHS with versus without SLE
Table 3: Outcomes of in-hospital DKA/HHS with versus without SLE
To cite this abstract in AMA style:
Chaisrimaneepan N, Yingchoncharoen P, Paz M. In-patient Outcomes of Diabetic Ketoacidosis and Hyperglycemic Hyperosmolar Syndrome in SLE: US National Inpatient Database (2021-2022) [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/in-patient-outcomes-of-diabetic-ketoacidosis-and-hyperglycemic-hyperosmolar-syndrome-in-sle-us-national-inpatient-database-2021-2022/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/in-patient-outcomes-of-diabetic-ketoacidosis-and-hyperglycemic-hyperosmolar-syndrome-in-sle-us-national-inpatient-database-2021-2022/
