Session Information
Date: Tuesday, October 28, 2025
Title: (2377–2436) Systemic Lupus Erythematosus – Diagnosis, Manifestations, & Outcomes Poster III
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Systemic lupus erythematosus (SLE) is a multisystemic chronic disease characterized by a wide range of clinical and serological manifestations. It most commonly affects young women, with incidence and disease activity typically declining with age. As a result, data regarding the diagnoses of SLE in individuals ≥60 years of age (elderly onset SLE) is scarce. To better characterize elderly-onset SLE, a multi-racial cohort of SLE patients was analyzed.
Methods: This analysis leverages a cohort of 1141 SLE patients who met SLE criteria by at least one method: American College of Rheumatology (ACR), Systemic Lupus Erythematosus International Collaborating Clinics (SLICC), and/or 2019 ACR/European League Against Rheumatism (EULAR) classification criteria. Lupus manifestations at the time of diagnosis were compared between elderly-onset SLE patients and those diagnosed at < 60 years old. An analysis of SLE presentation and diagnosis was conducted for elderly-onset SLE patients, including whether SLE diagnoses occurred during hospitalization, following referral to a rheumatologist, or through ongoing rheumatology clinic follow-up.
Results: Of 1141 patients with SLE, 90% were female and 10% were male. The racial and ethnic composition was as follows: 30% Black, 26% Hispanic, 22% White, 16% Asian, and 5% of unknown race/ethnicity. Within this cohort, 43 individuals were diagnosed at age ≥60 years (3.8%), while 1,098 were diagnosed at age < 60 years (96.2%). Additionally, there was a trend toward men being more likely to be diagnosed at age ≥60 years compared to those under 60 (19% vs. 10%, p=0.06). Among the 43 elderly-onset SLE patients, 9 were diagnosed between the ages of 65-69 and 10 were diagnosed at age ≥ 70, with the oldest being 82 years old. In this group, 28% had lupus nephritis (LN), with 6 patients later confirmed by a kidney biopsy. Compared to the remainder of the cohort, elderly-onset SLE patients exhibited significantly lower frequencies of malar rash at presentation (12% vs. 41%, p=0.0001), arthritis (33% vs. 69%, p ≤0.0001), and lupus nephritis (28% vs. 50%, p=0.004. (Table 1.) A majority of patients were diagnosed with SLE during hospitalization (47%), with 80% presenting with lupus-related complaints, and 20% presenting for SLE-unrelated issues (Table 2). The remaining diagnoses were made following referrals from a primary care physician or general rheumatologist (44%), with 11% of these referrals seeking evaluation for conditions other than lupus (Table 3).
Conclusion: This analysis identifies a distinct clinical profile in elderly-onset systemic lupus erythematosus (SLE). Despite immunosenescence, nearly 30% developed lupus nephritis (LN), with almost half diagnosed during hospitalization following severe symptom onset. Only one of 12 LN cases was referred by a rheumatologist for proteinuria; in most, renal involvement was recognized only after diagnosis of other SLE manifestations. These findings suggest new onset SLE and LN may be underrecognized in the elderly, leading to delayed diagnosis and increased disease severity.
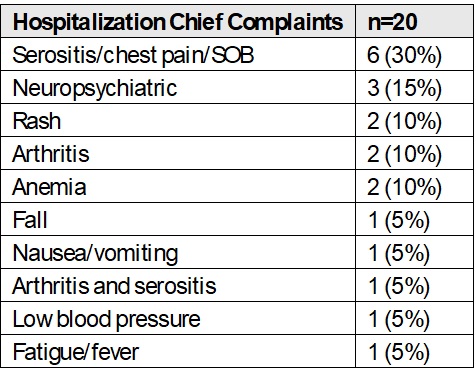 Table 1. Lupus clinical criteria profile for elderly-onset patients and patients diagnosed < 60 years of age
Table 1. Lupus clinical criteria profile for elderly-onset patients and patients diagnosed < 60 years of age
.jpg) Table 2. Hospitalization chief complaints in elderly-onset lupus patients
Table 2. Hospitalization chief complaints in elderly-onset lupus patients
.jpg) Table 3. Reasons for rheumatology referrals in elderly-onset lupus patients
Table 3. Reasons for rheumatology referrals in elderly-onset lupus patients
To cite this abstract in AMA style:
Dai J, Carter E, Masson M, Saxena A, Belmont H, Izmirly P, Buyon J. Clinical features of Elderly-onset Systemic Lupus Erythematosus [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/clinical-features-of-elderly-onset-systemic-lupus-erythematosus/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/clinical-features-of-elderly-onset-systemic-lupus-erythematosus/
