Session Information
Date: Tuesday, October 28, 2025
Title: (2227–2264) Rheumatoid Arthritis – Diagnosis, Manifestations, and Outcomes Poster III
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: The risk of interstitial lung disease is well established in Rheumatoid Arthritis (RA). Less is known about the airway involvement which has been estimated to occur in 39% to 60%, varying according to populations and investigative tools [1]. Small airways are defined as non-cartilaginous airways with an internal diameter less than 2 mm, and are characterized by lesions affecting the smallest bronchi and bronchioles [2]. Pulmonary function tests (PFT) are commonly used to measure small airway disease (SAD) but impulse oscillometry (IOS) appears as an innovative technique to more accurately determine SAD. IOS is a very sensitive measure of airway resistance particularly developed in asthma. This latter tool has never been used so far in RA patients.We sought to explore the distribution of key PFT and IOS features and the structure of their interrelationship in a cohort of RA patients
Methods: Included patients were followed for RA, with the exclusion of those with documented ILD. They were offered screening for RA airway using chest computed tomography (CT), PFT, and iOS. SAD involvement on CT was assessed by expert radiologists. Mosaic perfusion and expiratory air trapping were considered indicative of SAD.Key parameters from forced spirometry, body plethysmography, diffusing lung capacity for carbon monoxide, and IOS were obtained RA patients without known ILD. Hierarchical clustering and correlation network analysis were performed. Distal airway involvement is assessed using iOS with the R5-R20 parameter, where a value > 0.07 kPa/L/s indicates small airway disease [3].
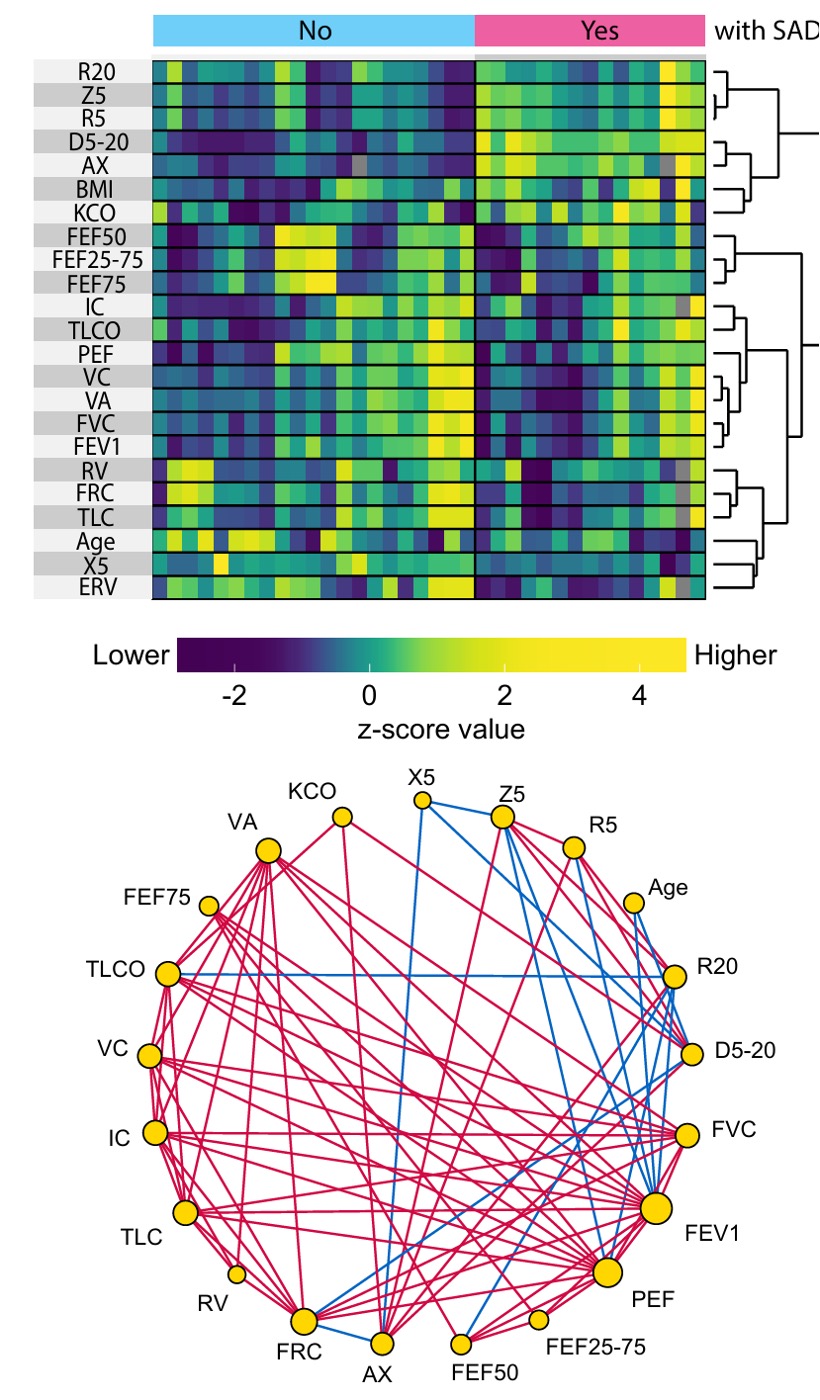
Results: The study population included 36 patients with RA (78% of female, mean age of 61.5 ± 10.5 y-o). A history of smoking was reported in 64% of patients. Seropositivity for rheumatoid factor and/or anti-citrullinated protein antibodies (ACPA) was observed in 97% of cases. At the time of inclusion, 44% of patients were receiving biologic DMARDs, mainly TNF inhibitors (9/36 patients). Respiratory symptoms (cough and/or dyspnea) or abnormal lung auscultation were present in 14% of patients. CT scans revealed SAD in 4 patients and ILD was observed in 5 out of 36 patients, predominantly with a pattern consistent with NSIP (3/5). Visually the data structure (Figure) showed that each PFT modality independently contributed to identify respiratory physiological status in RA. Although most PFT outcomes stayed within normal limits, the overall distribution clearly differentiated patients with SAD (n=15, 42%) from those without (n=21). The correlation network (Figure) revealed a robust interrelationship pattern among 20 PFT parameters, identifying 74 statistically significant correlations, predominantly positive (60 links), with 50 exhibiting strong correlations (r > 0.5).
Conclusion: Lung involvement appears as one of the key extra-articular damages occurring in RA. Beyond the risk of ILD, combined PFT and IOS can be efficient and complementary for detection of SAD in RA patients. This is offering a valuable strategy for identifying accurately subclinical respiratory involvement. Further studies are needed to clarify the prevalence, the prognosis and the management of SAD in RA.
To cite this abstract in AMA style:
HILLIQUIN S, HUA H, Pham-Ngoc H, Aubourg F, Lê-Dông N, Günther S, ROCHE N, AVOUAC J, Allanore Y, Dinh-Xuan A. Assessment of small airway disease in rheumatoid arthritis [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/assessment-of-small-airway-disease-in-rheumatoid-arthritis/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/assessment-of-small-airway-disease-in-rheumatoid-arthritis/