Session Information
Date: Tuesday, October 28, 2025
Title: (2195–2226) Reproductive Issues in Rheumatic Disorders Posters
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Systemic lupus erythematosus (SLE) increases the risk of placenta-mediated adverse pregnancy outcomes (APO) and may impact offspring cardiovascular health. Transplacental maternal anti-Ro antibodies can affect fetal cardiac function, while hydroxychloroquine (HCQ), though protective against APO, has been linked to cardiotoxicity in adults at high cumulative doses. Speckle tracking echocardiography (STE), a sensitive tool for detecting early cardiac dysfunction, remains underused in neonates. We used STE to assess the influence of maternal anti-Ro antibodies, gestational cumulative HCQ exposure, and APO on neonatal myocardial strain.
Methods: Participants were recruited from the Montreal site of the Lupus prEGnAnCY (LEGACY) cohort, a multicenter prospective cohort enrolling SLE pregnancies at < 17 gestational weeks. APO was evaluated at each trimester and postpartum, and included: 1) gestational hypertension, preeclampsia and/or eclampsia, 2) placental insufficiency, 3) placental abruption, and/or 4) small for gestational age (SGA < 5th percentile). Neonatal cardiac function was assessed ≤4 weeks postpartum using STE, with global longitudinal strain (GLS) reported via apical endocardial GLS or apical four-chamber peak longitudinal strain. GLS is expressed as a negative percentage, with more negative values indicating better myocardial contractile function. We summarized maternal and neonatal characteristics using descriptive statistics and evaluated GLS with univariable and multivariable regression analyses.
Results: This study included 26 pregnant women with SLE (each with a singleton pregnancy), of mean maternal age 35.9 ± 4.7 years and disease duration 9.9 ± 7.4 years. Most were in Lupus Low Disease Activity State (LLDAS) at baseline (85%), and 65% (15/26) maintained LLDAS throughout pregnancy. Live birth occurred in 89% (23/26) and fetal death in 11% (3/26). APO occurred in 42% (11/26), including gestational hypertension (15%), preeclampsia (23%), placental insufficiency (8%), placental abruption (8%), and SGA < 5th percentile (12%). Among 23 live births, 3 missed the STE assessment and 4 had suboptimal images preventing GLS estimation. Thus, GLS was assessed in 16 neonates of mean age 11.8 ± 26.2 days at STE. HCQ was used by all mothers (16/16), with mean cumulative gestational exposure of 1103.2 ± 294.6 mg x days/kg. Mean GLS was -26.3 ± 4.2%, with term neonates at -26.2 ± 4.3%. Lower mean GLS was observed in neonates born to mothers with APO (-25.2 ± 4.3%), anti-Ro antibodies (-24.8 ± 4.5%), and cumulative HCQ exposure in highest quartile (-24.6 ± 5.2%) versus their respective counterparts (-27.2 ± 4.1%, -27.9 ± 3.4%, and -28.2 ± 3.1%). GLS was not significantly associated with cumulative HCQ exposure, APO, or anti-Ro positivity in multivariable models adjusting for neonatal age and birth weight.
Conclusion: We observed lower GLS in neonates born to SLE mothers with anti-Ro antibodies and those with APO. Though not statistically significant, potentially due to small sample size, the trends may reflect subclinical cardiac alterations. These findings support the need for larger studies to clarify the impact of maternal antibodies, APO, and HCQ on fetal cardiac health.
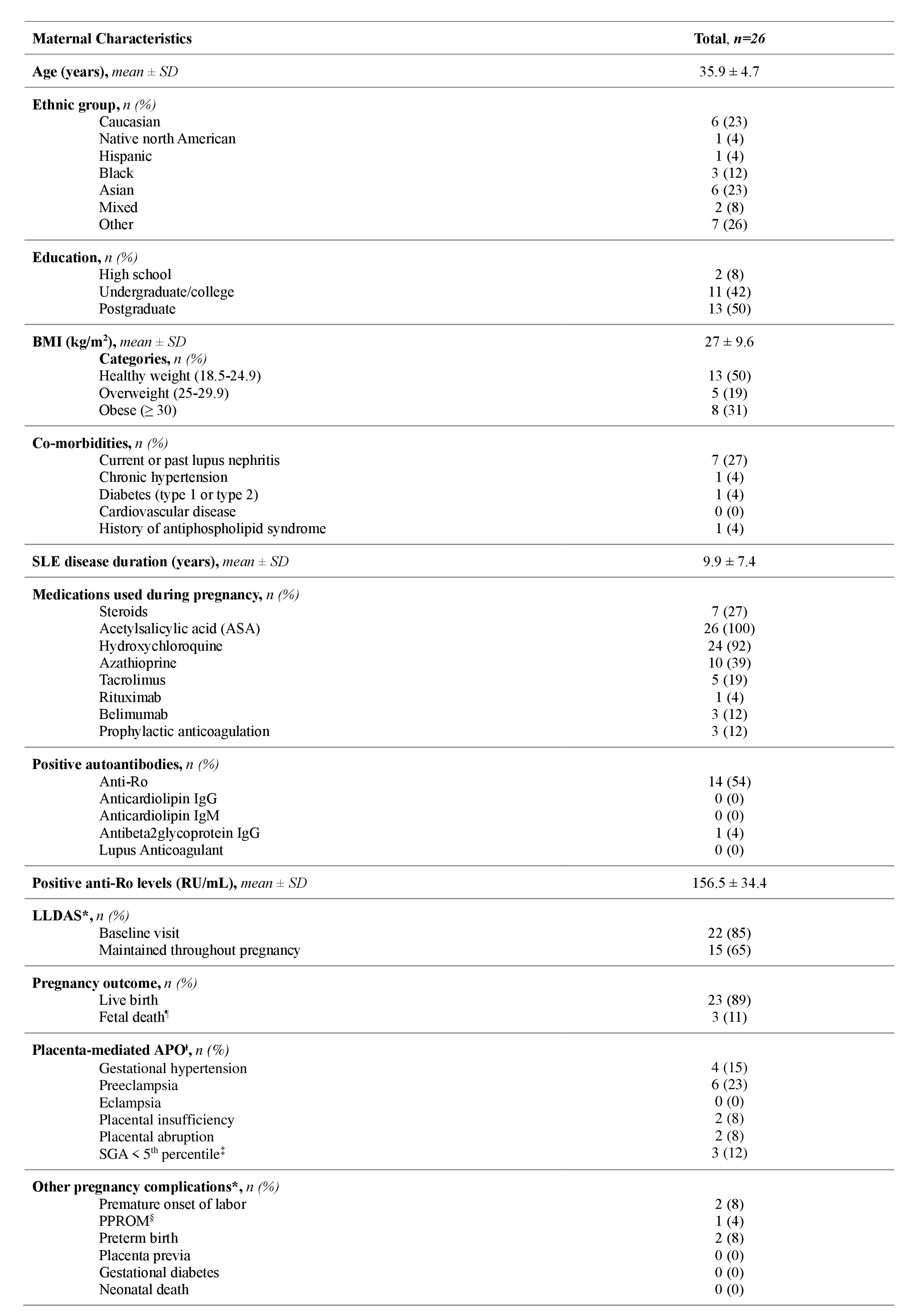 Table 1. Maternal and pregnancy characteristics.
Table 1. Maternal and pregnancy characteristics.
* LLDAS: Lupus Low Disease Activity State defined as 1) SLEDAI-2K score ≤ 4, with no activity in major organ systems (renal, CNS, cardiopulmonary), and no hemolytic anemia or gastrointestinal activity, 2) no new features of lupus disease activity compared to the previous assessment, 3) Physician Global Assessment (PGA) ≤ 1, 4) prednisone (or equivalent) dose ≤ 7.5 mg/day, and 5) the patient is on standard immunosuppressive drugs and/or biologics, including antimalarials, at well-tolerated, maintenance doses.
¶ Fetal death < 20 gestational weeks
Ɨ Placenta-mediated adverse pregnancy outcome: defined as a composite measure including: 1) gestational hypertension, preeclampsia and/or eclampsia, 2) placental insufficiency (i.e. Doppler flow suggestive of fetal hypoxemia, oligohydramnios, and/or relevant pathology), 3) placental abruption, and/or 4) SGA ( < 5th percentile).
‡ SGA: small for gestational age < 5th percentile
§ PPROM: Preterm premature rupture of membranes
.jpg) Table 2. Neonatal characteristics (n=16)
Table 2. Neonatal characteristics (n=16)
*HCQ: hydroxychloroquine
.jpg) Table 3. Neonatal global longitudinal strain (GLS) according to maternal and neonatal characteristics
Table 3. Neonatal global longitudinal strain (GLS) according to maternal and neonatal characteristics
To cite this abstract in AMA style:
Farhat R, Rudski L, Dayan N, Henin C, Villegas Martinez D, Sahussarungsi S, Kanaprach P, Bernatsky S, Altit G, Vinet E. Neonatal Myocardial Strain in Offspring born to Mothers with Systemic Lupus Erythematosus: Pilot Data from the LEGACY Cohort [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/neonatal-myocardial-strain-in-offspring-born-to-mothers-with-systemic-lupus-erythematosus-pilot-data-from-the-legacy-cohort/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/neonatal-myocardial-strain-in-offspring-born-to-mothers-with-systemic-lupus-erythematosus-pilot-data-from-the-legacy-cohort/
