Session Information
Date: Tuesday, October 28, 2025
Title: (2195–2226) Reproductive Issues in Rheumatic Disorders Posters
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Few studies exist that examine pregnancy outcomes in adolescents with SLE. To our knowledge, there have been no studies comparing SLE adolescent pregnancies to both adolescent control and adult SLE pregnancies. Using a de-identified electronic health record (EHR), we compared rates of pregnancy outcomes in adolescents ≤ 21 years with and without SLE to older individuals with SLE.
Methods: We identified SLE pregnancies in a de-identified EHR with >3.8 million individuals using a validated algorithm of ≥ 4 SLE ICD billing codes and ≥ 1 pregnancy or delivery codes. On chart review, we confirmed SLE diagnosis by a rheumatologist and excluded deliveries occurring before SLE diagnosis. Pregnancies at a maternal age ≤ 21 years were counted as adolescent pregnancies and pregnancies at a maternal age ≥ 22 years were considered adult pregnancies. We identified control individuals as those without ICD codes for autoimmune diseases and ≥ 1 pregnancy or delivery codes. Maternal outcomes included gestational diabetes, preeclampsia, postpartum hemorrhage, peripartum infection. Fetal outcomes were pregnancy loss, which included elective termination, spontaneous abortion, and stillbirth. Other fetal outcomes were premature birth, defined as delivery < 37 weeks, and small for gestational age, defined as birth weight < 10th percentile for gestational age. Covariates were assessed on chart review. Using Chi-square and Kruskal-Wallis tests, we compared demographics and pregnancy outcomes. Since individuals could contribute multiple pregnancies and parity can impact outcomes, we performed mixed effects models to estimate the association of pregnancy loss, preterm birth, and preeclampsia with age at delivery, race, and SLE case status.
Results: We identified 32 pregnancies to 27 individuals with SLE ≤ 21 years, 146 pregnancies to 90 adolescent control individuals without SLE, and 266 pregnancies to 182 individuals with SLE aged ≥ 22 years (Table 1). Adults with SLE were more likely to be White than adolescents with or without SLE (p < 0.001), and SLE pregnancies were more likely to be complicated by hypertension compared to controls (p < 0.001). Compared to adolescent control pregnancies, adolescent SLE pregnancies were more likely to experience preeclampsia (p < 0.001), postpartum hemorrhage (p = 0.001), and preterm delivery (p = 0.001). Among SLE pregnancies, SLE adolescents were more likely to have antiphospholipid antibody syndrome (p = 0.01) and nephritis (p = 0.001) compared to SLE adults. Adolescents with SLE were more likely to have pregnancy loss than adults with SLE (p = 0.02). In mixed effects models, SLE cases were more likely to experience preterm delivery (OR = 9.11, 95% CI 4.10-20.22) and preeclampsia (OR = 5.55, 95% CI 2.38 – 12.92) after adjusting age at delivery and race.
Conclusion: Adolescent SLE pregnancies were more likely to have preterm birth, preeclampsia, and post-partum hemorrhage than control adolescents and more likely than adults with SLE to have pregnancy loss. Adolescents with SLE represent a high-risk pregnancy group that needs close monitoring.
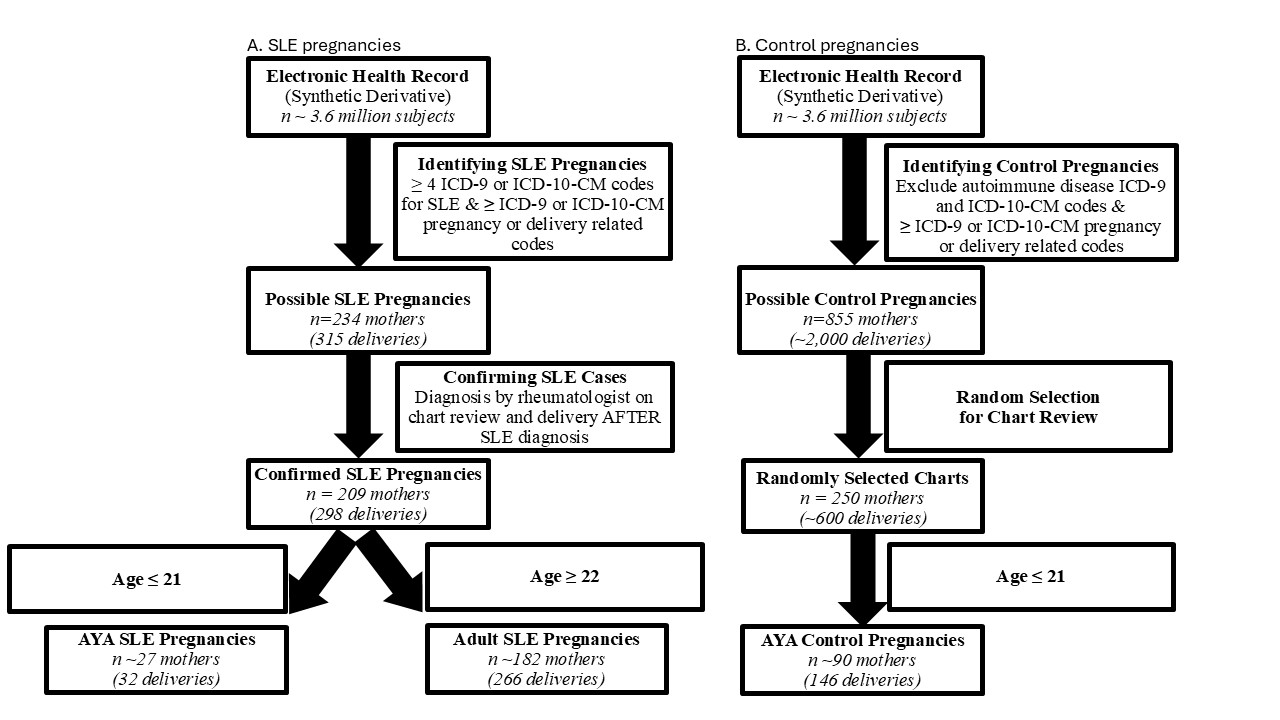 Figure 1. Flowchart of study individuals. (A) SLE pregnancies were selected from the de-identified electronic health record (EHR) using four or more SLE ICD-9 or ICD-10-CM
Figure 1. Flowchart of study individuals. (A) SLE pregnancies were selected from the de-identified electronic health record (EHR) using four or more SLE ICD-9 or ICD-10-CM
codes while also requiring one or more ICD-9 or ICD-10-CM pregnancy or delivery-related codes. We then performed chart review to confirm SLE diagnosis by a rheumatologist and ensure pregnancy occurred after SLE diagnosis. After applying age criteria, we identified adolescent SLE pregnancies and adult SLE pregnancies. (B) Control pregnancies were selected from the same de-identified EHR as the SLE pregnancies. Controls were required to have the same pregnancy and delivery-related codes used for SLE deliveries and to not have ICD-9 or ICD-10-CM codes for autoimmune diseases. We then performed chart review on a random set of 250 controls to ensure no autoimmune diseases. After applying age criteria, we identified adolescents without SLE.
To cite this abstract in AMA style:
Deffendall C, Green S, Suh A, Han B, Barnado A. Adolescents with Systemic Lupus Erythematosus at Highest Risk of Adverse Pregnancy Outcomes [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/adolescents-with-systemic-lupus-erythematosus-at-highest-risk-of-adverse-pregnancy-outcomes/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/adolescents-with-systemic-lupus-erythematosus-at-highest-risk-of-adverse-pregnancy-outcomes/

.jpg)
.jpg)